Quality Improvement Programs: Hurdles to Optimizing Care
Many QI programs are subject to missteps, but approaches that implement QI essentials can bring healthcare closer to realizing its potential.
- By BSTQ Staff
THE HEALTH RESOURCES and Services Administration defines quality improvement (QI) as the systematic and continuous actions that lead to measurable improvement in healthcare services and the health status of targeted patient groups.1 At first glance, QI seems like a straightforward concept: Use practices that improve the quality of care provided, and minimize or eliminate those that have the opposite effect. In other words, provide healthcare in keeping with The Institute of Medicine’s definition: “The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”2
QI can confer numerous benefits:3
- Helping organizations prepare for the transition to value-based payment models
- Allowing organizations to participate in the public reporting of physician-quality data
- Giving organizations the opportunity to participate in federal QI incentive programs
- Equipping organizations with the skills necessary to apply for and complete national recognition programs
Several elements are fundamental to QI, including establishing a culture of quality, determining and prioritizing potential areas for improvement, collecting and analyzing data, communicating results and committing to ongoing evaluation.3
Unlike quality assurance programs, which are reactive and retrospective, QI programs are both retrospective and prospective. Their purpose is to help an organization determine its status and evaluate ways to improve.4
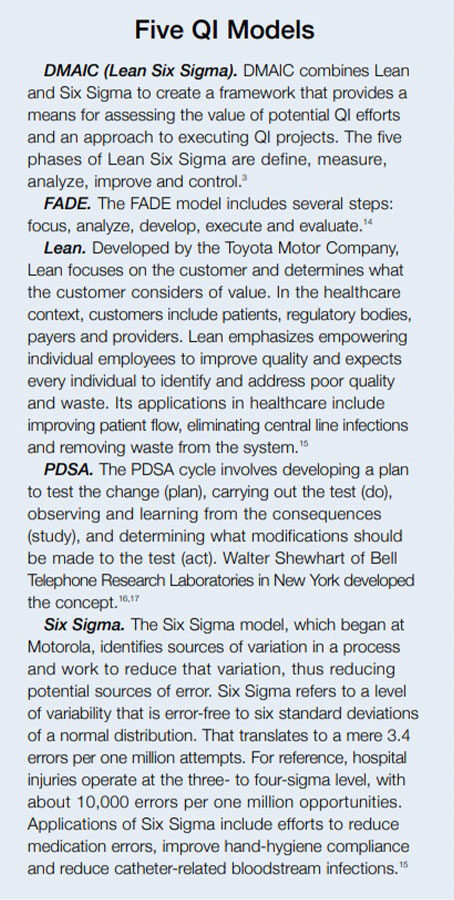
QI programs are used widely in healthcare. Numerous agencies and organizations, such as the Agency for Healthcare Research and Quality, The Joint Commission and the National Quality Forum, are dedicated to providing better care using numerous process improvement models such as DMAIC, FADE, Lean, PDSA and Six Sigma (see Five QI Models).5 Yet, with resources in place, and so many QI programs being implemented, it is still difficult for healthcare to realize its full potential.6
The Case for Improving QI
Paul Batalden, active emeritus professor at Dartmouth College’s Geisel School of Medicine, and Frank Davidoff, adjunct professor of The Dartmouth Institute and executive editor at the Institute for Health Improvement, define QI as “the combined and unceasing efforts of everyone — healthcare professionals, patients and their families, researchers, payers, planners and educators — to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development (learning).” They add that change-making must become an intrinsic part of everyone’s job “every day, in all parts of the system.”6
The two warn that not all changes are improvement. To avoid pitfalls of changes that aren’t beneficial, they argue that change should be driven by generalizable scientific evidence that is systematically incorporated. In addition, settings in which care is delivered need to be characterized. And, to know that improvement is occurring, accurate and powerful measurements of what is happening are needed.6 These emphases lead to better knowledge, but it still takes people on all levels to effect change using that knowledge. “It is one thing to expect a specially commissioned ‘QI team’ to be actively engaged in designing and testing the many changes needed for better patient and population outcomes, better system performance and better professional development; it is quite another to expect everyone involved in healthcare to do so, and do so all the time,” they write.
QI Missteps
Believing technology has all the answers. “Somewhere near 80 percent of your system’s data exists outside your EMR [electronic medical record] or ERP [enterprise resource planning] system. That means operational and clinical decisions are being made with only a fraction of the available data,” according to Conduent, a business process services company. In short, keeping accurate digital records is critical, but it’s not the whole story in terms of healthcare delivery. Unstructured data, such as that which resides in free-text or semi-structured documentation, is as important as that found in the electronic record.7,8
Unstructured data capture often arises to avoid hindering the healthcare-delivery process, according to Dan LeSueur, senior vice president of technical operations at Health Catalyst, a data warehousing, analytics and outcomes-improvement company for the healthcare industry. “As a result,” he writes, “much of the data captured in this manner is difficult to aggregate and analyze in any consistent manner.”9
Adopting a “work-harder” approach. The work-harder approach to QI assumes employees must do more with the same time, resources and supports. “Many recent quality improvement initiatives have counted on the healthcare workforce, especially staff at the point of care, to implement the desired changes, effectively layering additional workload on an already busy environment, complex and generally inefficient system,” write Batalden, Christopher Hayes, associate scientist at the Li Ka Shing Knowledge Institute in Toronto, and Donald Goldmann, professor at Harvard School of Public Health and senior physician at Boston Children’s Hospital.10
Nurses may be required to do more work because important (but time-consuming) steps have been added to their routines. Tasks such as patient intake may take front office staff longer after improved procedures have been identified and adopted. In the work-harder model, employees have more to do and less time to do it. Their accuracy and reliability may decrease, or they may pay less attention to other tasks — or to patients.10
Hayes, Batalden and Goldmann say there is ample evidence that the work-harder approach leads to change fatigue, resistance, cynicism, burnout and turnover.
Forgetting the patient. Perhaps the most important item on the misstep list is leaving the patient out of the QI program. Meeting the needs and expectations of patients is a central aspect of QI. Patient safety, coordination of care within the larger healthcare system, and cultural competence are just a few of the patient-oriented services that QI can address.1,7
Other issues. Several other mistakes can undermine QI initiatives. Two that fall under the banner of “not all change is good change” are reinventing the wheel and throwing out what’s working. Additional errors include underestimating change management, not being clear about the desired state, conflating strategy and execution, failing to align the business and clinical sides of the organization, waiting for government to design change, and using a bottom-up approach.7
QI Essentials
Having strong leadership. Ronda G. Hughes, senior health scientist administrator at the Agency for Healthcare Research and Quality, says the importance of having strong leadership commitment and support cannot be overstated. “Without the commitment and support of senior-level leadership, even the best intended projects are at great risk of not being successful,” she says.11
Peter Lachman, deputy medical director for safety at Great Ormond Street Hospital in London, agrees. He says a new approach to leadership is needed for successful QI. “There needs to be a change in the mental model of leadership in which one talks about patients as partners,” he explains. “One talks about listen [sic] to the front line and understand what it’s like to be on the front line.”
This requires a softening of the boundaries between different areas of healthcare, in particular those that typically work in isolation. “You have to break down the boundaries between different groups of professionals and between professionals themselves,” Lachman says. And, to be a quality leader, he says, one needs to understand QI methodology, as well as how to measure and how to question. In addition, leaders must know how to involve all kinds of people in the QI program.12
Clearly defining the project. Good programs start with a good sense of the problem. The problem statement should be defined at the outset, the vision should be clear, and the project scope should be defined. Covering these bases will allow everyone involved to know what the goal is and what to expect. Objectives should be clear and measurable. Deliverables and responsible parties should be spelled out. Resources should be allocated to ensure the project’s success.13
Including everyone in the process. Knowledge of what needs to improve is only half of QI. The other half is involving everyone from care providers to support staff in the process. “Drawing everyone actively into the process of testing change, all the time, presumes that everyone will develop a basic understanding of the standards of their work, as well as the skills they need to test changes in that work,” Batalden and Davidoff write. “Making improvement happen also requires leadership that enables connections between the aims of changes and the design and testing of those changes; that pays serious attention to the policies and practices of reward and accountability; and unshakeable belief in the idea that everyone in healthcare really has two jobs when they come to work every day: to do their work and to improve it.”6
Other essentials. Additional elements of successful QI include having a culture of safety and improvement, understanding the problem and its root causes, using a methodologically sound approach, standardizing care processes, keeping plans flexible and recognizing that change takes time.11
Better Care Is Possible Despite the hurdles of QI, achieving better care is possible. The best approaches to QI avoid many of the pitfalls by understanding what areas need to be improved before committing to a QI program, including staff at all levels and committing to ongoing evaluation of change initiatives to ensure they are, in fact, beneficial.
References
- Health Resources and Services Administration. Quality Improvement. Accessed at www.hrsa.gov/quality/ toolbox/508pdfs/qualityimprovement.pdf.
- National Institutes of Health. HSRIC: Quality. Accessed at www.nlm.nih.gov/hsrinfo/quality.html.
- American Academy of Family Physicians. Basics of Quality Improvement. Accessed at www.aafp.org/practice-management/ improvement/basics.html.
- Duke University School of Medicine. What Is Improvement? Contrasting QI and QA. Accessed at patientsafetyed.duhs.duke.edu/module_a/introduction/contrasting_qi_qa.html.
- Duke University School of Medicine. What Is Quality Improvement? Accessed at patientsafetyed.duhs.duke.edu/module_a/introduction/introduction.html.
- Batalden P and Davidoff F. What Is “Quality Improvement” and How Can It Transform Healthcare? BMJ Quality and Safety, 2007;16:2-3. Accessed at qualitysafety.bmj.com/content/16/1/2.full.
- Conduent. 10 Common Mistakes in Healthcare Provider Process Improvement. Accessed at www.conduent.com/insights/healthcare-provider-solutions/process-improvement.
- HIT Consultant. Why Unstructured Data Holds the Key to Intelligent Healthcare Systems. Accessed at hitconsultant.net/2015/03/31/tapping-unstructured-data-healthcares-biggest-hurdle-realized.
- LeSueur D. 5 Reasons Healthcare Data Is Unique and Difficult to Measure. Health Catalyst. Accessed at www.healthcatalyst.com/5-reasons-healthcare-data-is-difficult-to-measure.
- Hayes C, Batalden P, and Goldmann D. A “Work Smarter, Not Harder” Approach to Improving Healthcare Quality. BMJ Quality and Safety, 24(2), 100–102. Accessed at qualitysafety.bmj.com/content/24/2/100.full.
- Hughes R. Tools and Strategies for Quality Improvement and Patient Safety. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses (1146–1168). Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. Accessed at www.ncbi.nlm.nih.gov/books/NBK2682.
- Lachman P. Expert Interview: Peter Lachman, Key Ingredients for Quality Improvement, Oct. 9, 2015. Accessed at www.youtube.com/watch?v=fzBqZZoIJUE.
- Parker J. 10 Keys for Successful Process Improvement Programs (Part 1). EnFocus Solutions. Accessed at enfocussolutions.com/10-keys-for-successful-process-improvement-programs-part-1.
- Duke University School of Medicine. What Is Quality Improvement? Methods of Quality Improvement. Accessed at patientsafetyed.duhs.duke.edu/module_a/methods/methods.html.
- Glasgow J. Introduction to Lean and Six Sigma Approaches to Quality Improvement. Agency for Healthcare Research and Quality. Accessed at www.qualitymeasures.ahrq.gov/expert/expert-commentary/32943/introduction-to-lean-and-six-sigma-approaches-to-quality-improvement.
- Institute for Healthcare Improvement. Plan-Do-Study-ACT (PDSA) Worksheet. Accessed at www.ihi.org/resources/pages/tools/plandostudyactworksheet.aspx.
- The W. Edwards Deming Institute. PDSA Cycle. Accessed at deming.org/management-system/pdsacycle.