Breakthroughs in the War on Cancer
As the number of cancer cases continues to rise, scientists are bringing to light exciting discoveries that are being used to create targeted therapies to treat and, it is hoped, to eventually cure cancer.
- By Ronale Tucker Rhodes, MS
NEARLY 40 PERCENT of men and women will be diagnosed with cancer at some point during their lifetime, according to the National Cancer Institute’s Surveillance, Epidemiology and End Results Program. In 2013, an estimated 14,140,254 people were living with cancer in the U.S. In 2016, the estimated number of new cases is predicted to be 1,685,210, resulting in approximately 595,690 deaths.1
No doubt, cancer is big business. IMS Health, a global information and technology services company, reports global oncology sales exceeded $107 billion in 2015, and forecasts growth between 7.5 percent and 10.5 percent through 2020, reaching $150 billion. In just the past five years, more than 70 new cancer treatments have been launched.2 Understandably, it’s not just dollars at stake; it’s the lives of the millions of patients who are counting on those billions of dollars spent in cancer care research to produce new and innovative drugs to combat the terrifying statistics. “The new science redefining cancer as a large number of narrowly defined diseases and yielding therapeutic options for an expanding number of patients is rapidly transforming the oncology treatment landscape,” said Murray Aitken, IMS Health senior vice president and executive director of the IMS Institute for Healthcare Informatics. “Most health systems are struggling to adapt and embrace this evolution — including the regulatory systems, skilled professionals, diagnostic and treatment infrastructures, and financing mechanisms that are required to serve the needs of cancer patients around the world. These challenges deserve urgent attention in light of the strong near-term pipeline of clinically distinctive therapies and new programs such as the U.S. government’s ‘cancer moonshot’ that are galvanizing research efforts to change the trajectory of cancer.”2
These clinically distinctive therapies are a result of several cutting-edge areas of research and care: targeted therapies that include immunotherapy, combination therapies, vaccines and genomics — all of which are designed to block the growth and spread of cancer.
The Houdini of Cancer
There is, of course, a reason why cancer is so difficult to treat and why researchers have yet to find a cure after all this time (the first case of cancer dates back to 1500 B.C.3): Every patient’s cancer is unique. According to professor Gerard Evan, head of the department of biochemistry at the University of Cambridge conducting a study of the genes that drive the development and growth of cancer, called oncogenes, “Cancers develop through the buildup of mutations (errors) in the genes that regulate and restrain the growth, division and movement of the cells that make up our bodies … and the cells then either die out or survive and multiply as a result of the complex, changing and still largely mysterious selective pressures in the body.”4
Even with treatment, cancer cells adapt and evolve in response. “Even drugs that are initially very effective often have a progressively dwindling effect over time as the biological systems that are blocked by the treatment spontaneously compensate by rerouting the cancer cells’ internal wiring, thereby restoring the cancer’s ability to grow and spread,” explains Evan. “To use an analogy, traffic hot spots in towns can cause major traffic jams, but cunning drivers will quickly find shortcuts to get around the congestion.”4 In essence, cancer cells are like Houdini: They almost always seem to find a way out.
But, now, research is beginning to shed light on how cells escape past the immune system.
Researchers at Texas A&M College of Medicine found that when cancer cells are able to block the function of a gene called NLRC5, they are able to evade the immune system and proliferate. Biopsy samples from almost 8,000 cancer patients showed that the expression of the NLRC5 gene is highly correlated with cancer patient survival; patients who survive longer have greater expression of the gene. The discovery is significant, they say, because in the short term, it can more accurately predict how likely the tumor can be recognized and destroyed. And, in the long term, therapies could be developed that increase expression of the gene and use it to help fight cancer.5
In another study, a Kyoto University-led team found that structural changes affecting the regulation of the PD-L1 gene appear to help some cancers dodge the immune system. The team used genome and/or RNA sequence data for more than four dozen adult T-cell leukemia/lymphoma cases to search for noncoding structural variant clusters. What they found were structural variants in the 3’-untranslated region (UTR) of the PD-L1 that appeared to amplify the gene’s expression, apparently contributing to tumors’ ability to evade the immune system. Similar structural variant patterns were found in samples from individuals with diffuse large B-cell lymphoma and stomach adenocarcinoma. Follow-up experiments in a mouse model indicated that such 3’-UTR alterations can boost PD-L1 expression, prompting tumor protection from the immune system. The researchers then demonstrated that they could dial up PD-L1 expression by using CRISPR-Cas9 to interfere with the PD-L1 3’-UTR in mouse or human cell lines. Experiments on mouse models showed diminished immune responses to cancer-causing cells containing the truncations. Based on their findings, the team speculated that “disrupted PD-L1 3’-UTR might serve as a genetic marker for identifying cancers that actively evade immune surveillance and, therefore, potentially respond to immune checkpoint blockade using antibodies against PD-1/PD-L1.”6
In June, researchers from the United Kingdom discovered how two molecules join forces to help cancer cells survive as they metastasize. The finding occurred when they observed what happens when cancer cells break away from tumors in cell cultures, zebra fish and mice. They found that “integrins” (proteins on the surface of a cell that bind and communicate with its surroundings) play a role in cancer cells surviving after they detach from the primary tumor. Integrins are known to engage in “outside-in” and “inside-out” signaling, which helps cancer cells bind to their surrounding environment. But when cancer cells travel during metastasis, the integrins adopt “inside-in” signaling, causing a defense signaling to occur within the cell. According to the study’s authors, the integrin beta-1 (B1) teams up with a protein called c-Met, and both proteins travel together inside the cancer cell. The proteins then move to a location within the cell that is normally used for degradation and recycling of cell material. However, the proteins use this location to send a signal to other areas of the cancer cell, triggering a defense against cell death. The researchers then looked at what would happen if both B1 and c-Met were prevented from entering cells or from traveling to the location needed for defense signaling and then found that the cells were much less likely to metastasize. The findings suggest that stopping B1 from initially entering cancer cells could be an effective way to combat cancer metastasis.7
Most recently, researchers at the University of California, Los Angeles discovered key mechanisms in how melanoma becomes resistant to immunotherapy. In their study of 78 patients who were treated with pembrolizumab (Keytruda), 42 patients responded, but 15 patients relapsed. Of those 15, four met the study criteria. When analyzing pairs of tissue samples taken from the four individuals before starting treatment and after they relapsed, the researchers found that the post-relapse tumors were very similar to those of their initial tumors; however, some significant changes occurred that allowed the cancer to fight back. In one case, a tumor had lost the B2M gene, making it harder for T cells to recognize the cancer. In two other cases, genetic mutations in the tumors interfered with JAK1 and JAK2 genes, which limited the immune system’s effectiveness in killing cancer cells. The fourth patient’s tissue didn’t have those genetic alterations, suggesting that other mechanisms of resistance may be discovered in the future.8
Beyond Cytotoxic Therapies
Many different types of cancer therapies are available that differ from cytotoxic radiation and chemotherapy. Most promising are targeted therapy, immunotherapy, vaccines and gene therapy.
The U.S. Food and Drug Administration (FDA) has approved a great number of targeted therapies for more than a dozen types of cancer. In addition, there are ongoing clinical trials being studied for both FDA-approved and experimental targeted therapies for specific types of cancer. These trials can be located under the types of therapies at the National Cancer Institute (www.cancer.gov/about-cancer/treatment/clinical-trials/search) or by doing a search of a type of cancer at clinicaltrials.gov.9
Targeted Therapies: The Cornerstone of Precision Medicine
Drugs or other substances that block the growth and spread of cancer are one of the most promising new therapeutic strategies. Known as targeted therapies (a cornerstone of precision medicine that uses information about a person’s genes and proteins to prevent, diagnose and treat disease), they work by interfering with specific molecules that are involved in the growth, progression and spread of cancer. They differ from traditional chemotherapy because they 1) act on specific molecular targets that are associated with cancer, rather than acting on all rapidly dividing normal and cancerous cells; 2) are deliberately chosen or designed to interact with their target, rather than just killing cells; and 3) are often cytostatic, meaning they block tumor cell proliferation, rather than cytotoxic, meaning they kill tumor cells.
Several approaches are used to identify good targets. One is to compare the amounts of individual proteins in cancer cells with those in normal cells. An example of this is the human epidermal growth factor receptor 2 protein (HER-2), which is expressed at high levels on the surface of some cancer cells. A second approach is to identify potential targets to determine whether cancer cells produce mutant (altered) proteins that drive cancer progression. And, a third approach is to look for abnormalities in chromosomes that are present in cancer cells but not in normal cells, which can sometimes result in the creation of a fusion gene (one that incorporates parts of two different genes) whose product, called a fusion protein, may drive cancer development. All of these proteins are potential targets for targeted cancer therapies.9
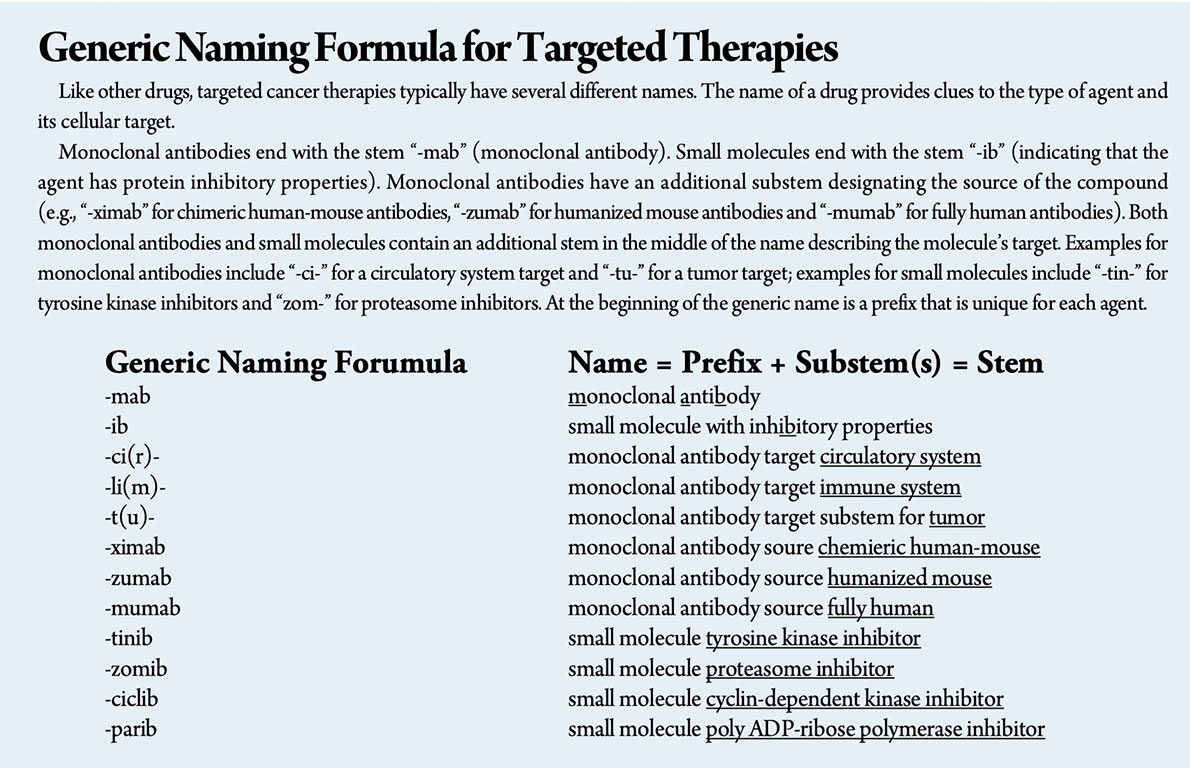
Targeted therapies are typically either small molecules or monoclonal antibodies. Small molecules can penetrate the cell membrane to interact with targets inside a cell, usually by interfering with the enzymatic activity of the target protein. Monoclonal antibodies target specific antigens found on the cell surface and, sometimes, they are conjugated to radioisotopes or toxins to allow specific delivery of the cytotoxic agents to the intended cancer cell target.
Unfortunately, as mentioned earlier, cancer cells adapt and evolve in response to treatment, causing them to become resistant to targeted therapies in two ways: mutating so that the targeted therapy no longer interacts well with it, and/or finding a new pathway to achieve tumor growth that doesn’t depend on the target. Therefore, many targeted therapies work best in combination with one or more traditional chemotherapy drugs.10
Immunotherapy: Using the Body’s Natural Defense System
While immunotherapy falls under the umbrella of targeted therapy, it differs because rather than aiming to inhibit molecular pathways that are crucial for tumor growth and maintenance, immunotherapy uses the body’s own natural defense system by stimulating a host immune response to achieve long-lived tumor destruction. Targeted therapies and cytotoxic agents such as chemotherapy and radiation also achieve immune responses, so treatment strategies often combine them.11
A growing number of studies are showing great success with targeted immunotherapies, both approved and experimental, for treating a host of diseases.
Melanoma. In 2015, former president Jimmy Carter announced he was cancer-free after being treated with the immune-boosting drug Keytruda (pembrolizumab, Merck). Now, a new study shows that an estimated 40 percent of 655 people treated with Keytruda in a clinical trial to treat advanced melanoma were still alive three years after starting treatment. The three-year survival rate with older melanoma treatments was only 10 percent to 20 percent.12
Another study showed that 34 percent of melanoma patients treated with Opdivo (nivolumab, Bristol-Meyers Squibb) were alive five years after starting treatment. In comparison, the overall survival rate for patients with advanced melanoma has been about 15 percent to 20 percent, according to the American Cancer Society.12
And, in a third Phase II study known as CheckMate-069 that examined the combination of Yervoy (ipilimumab, Bristol-Meyers Squibb) and Opdivo, there was a 42 percent improvement in overall survival when compared with Yervoy as a monotherapy.13
Bladder cancer. Opdivo has also been shown to be effective for treating metastatic bladder cancer. A Phase I/II clinical trial treated 78 patients, five of whom (6.4 percent) had complete responses, 14 (18 percent) of whom had partial responses in which tumor burden shrank by at least 30 percent, and 22 (28.2 percent) had stable disease. Thirty (38 percent) patients had disease progression.14
In May, FDA approved the first immunotherapy to treat bladder cancer. Tecentriq (atezolizumab, Genentech), which works in a similar way as Keytruda by targeting the PD-L1 protein, won accelerated approval for treating patients with advanced urothelial cancer after chemotherapy stops helping them — a point when most usually die within six months. Approval was based on a study of 310 people with advanced urothelial cancer, which found that treatment stopped tumors from growing in 24 percent of patients and shrank tumors by 30 percent.15
Stomach cancer. Recently, new research suggests that advanced stomach cancer patients may live longer with an IMAB362 antibody therapy. IMAB362 is an antibody that focuses on a protein on cancer cells known as claudin 18.2. In a Phase II clinical trial of 161 stomach cancer patients, those who received the treatment and standard chemotherapy survived about 13 months versus those who received only chemotherapy whose median survival was just 8.4 months. Participants with the highest levels of claudin 18.2 had even longer survival rates, with a median survival of 17 months.16
Brain cancer. In May, the National Brain Tumor Society and Oligo Nation granted $250,000 to fund a preliminary study of an immunotherapy to treat oligodendroglioma, a type of brain cancer. Researchers at Stanford University have developed an antibody that will target the CD47 protein that sends a “don’t eat me” signal to immune cells, thus hiding tumors from the innate immune system. Currently in Phase I studies for a number of solid tumors and blood cancers, the new study aims to determine if patients with oligodendroglioma can clinically benefit from anti-CD47 treatment. To date, results from lab tests have shown the method is effective. Researchers are now conducting studies based on three approaches: 1) testing anti-CD47 using multiple animal models; 2) conducting in vivo animal testing of the anti-CD47 antibody in combination with various immunotherapies, including EGFR inhibitors and anti-CD-40 agents; and 3) performing in vivo testing of the efficacy of combined immunotherapies that encourage an adaptive response from the immune system, including inhibitors (PD-1, PD-L1 and CTLA-4).17
Another new potential treatment for brain cancer is the poliovirus, and FDA has given it breakthrough status. The treatment, developed at Duke University, involves injecting a genetically engineered poliovirus, known as PVS-RIPO, into deadly brain tumors known as glioblastoma, a virulent cancer that kills approximately 12,000 Americans every year — 60 percent of whom die within two years of diagnosis. Early testing involving primates and human patients has found PVS-RIPO locates cancer cells and destroys them, without harming healthy tissues. Once brain tumors are infected with PVS-RIPO, a patient’s immune system recognizes and targets the virus infections and kills the cancer cells. The research is still in Phase I clinical trials, but since 2012, at least five patients have been treated. One 20-year-old woman who was treated is now cancer-free three years after the initial diagnosis.18,19
In July, researchers at the University of California, Los Angeles developed a new combination immunotherapy to treat glioblastoma, which works by preventing brain cancer cells from shielding themselves from a patient’s own immune responses. In a three-year study, they found that blocking the immune cell’s PD-1 surface receptors with antibodies in combination with a dendritic cell vaccine is more effective than either method used alone. PD-1 antibody blockade removes the shield that glioblastomas activate to hide from a patient’s immune system; however, the shield doesn’t activate a robust enough killer T cell response as the dendritic cell vaccine does. So, combining both the vaccine and antibody blockade provides a more effective immunotherapy.20
Lymphoma. In addition to its approval to treat melanoma and lung and kidney cancer, Opdivo also is now approved to treat Hodgkin’s lymphoma. FDA granted accelerated approval to Opdivo in May for classic Hodgkin’s lymphoma that has returned or progressed after a specific type of stem cell transplant and post-transplant medicine. In clinical trials of 95 patients with relapsed or refractory disease treated with Opdivo, tumors shrank in 65 percent of patients: 58 percent achieved partial remission, and 7 percent achieved complete remission. The median duration of response was 8.7 months.21
Researchers at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine are testing a cellular immunotherapy for treating patients with diffuse large B-cell lymphoma who have failed standard therapy. The investigational anti-CD19 chimeric antigen receptor T cell therapy, known as KTE-CD19, is being studied in a Phase II clinical trial for patients with aggressive non-Hodgkin’s lymphoma. In the trial, the patient’s own T cells are collected from peripheral blood and shipped to a special manufacturing facility where they are genetically engineered to display a novel receptor on their surface called a chimeric antigen receptor that enables the T cells to recognize a specific protein present on lymphoma cells called CD19. The modified cells are then returned and transfused back into the patient to target the lymphoma.22
Other cancers. An experimental drug is being tested in a small Phase Ib clinical trial to fight a variety of cancers. Pfizer’s utomilumab (the proposed nonproprietary name for PF05082566) targets the 4-1BB (also called CD137) agonist in combination with Keytruda, a PD-1 inhibitor, in patients with advanced solid tumors. Researchers are hopeful that combining the drugs, one that takes the brakes off the immune system with one that hits the accelerator, will offer long-lasting protection against cancer without adding serious side effects. In the trial of 23 patients with advanced pancreatic, colorectal, kidney, thyroid and two major forms of lung cancer, six experienced complete or partial responses, and one patient with small cell lung cancer and one with kidney cancer experienced complete remission. Utomilumab has already shown encouraging early results against a form of blood cancer when used with Roche’s Rituxan.23
Also being studied is an immune-strengthening compound combined with radiation therapy to extend the immune response that the radiation therapy induces so that both irradiated tumor sites and tumors outside the radiation field are affected. Researchers treated mice with radiation in combination with L19-IL2, a combination of an antibody that targets tumor blood vessels and a cytosine, a small protein involved in cell signaling in the immune system. After treatment, mice were tumor-free. In addition, when the treated mice were re-injected with cancer cells 150 days after treatment, they did not form new tumors. In contrast, 100 percent of untreated mice formed new tumors.
There was also an increase in the number of cells with an immunological memory. A Phase I/II clinical study in humans has been started to look at the combination treatment in patients with oligometastic solid tumors.24
Using the Body to Fight Cancer: The Power of Cells and Proteins
Researchers are also making new discoveries that explain why some therapies don’t work as well as they should, and that could provide potential for targeted immunotherapies.
Scientists at Dana-Farber Cancer Institute have developed a new approach that incites an immune system attack on tumors by changing the identity of key immune system cells dispersed throughout the tumor. Known as T regulatory (Treg) cells, they ordinarily prevent the more combative T effector (Teff) cells from attacking the tumor. But, researchers showed that eliminating a key protein in Tregs makes them so unstable that they become Teffs and join in destroying the tumor. While conversion from Tregs to Teffs occurs only in the inflammatory conditions that prevail in many tumors, when embedded in normal tissue through the body, Tregs continue to have a restraining effect on their local Teffs, which protects healthy organs from attack. A previous study showed that Tregs maintain their immune-suppressive properties under inflammatory conditions as long as they have high enough levels of a protein called Helios. When deprived of sufficient Helios, Tregs lose stability and turn into Teffs.
In the study, researchers explored whether converting Tregs to Teffs could be harnessed for therapeutic purposes in cancer. In the first experiment, they injected melanoma or colon cancer cells in mice engineered to lack Helios in their Treg cells and found that they developed tumors far more slowly than did animals with normal Treg cells. “Inspection of the animals’ tumor tissue showed an unstable set of T regulatory cells, many of which had converted into Teffs,” said senior author Hye-Jung Kim, PhD. They then explored whether stopping Helios production in tumor-dwelling Tregs could have the same effect by testing several antibodies that bind to key receptors on Tregs and cause a downturn in Helios production. Choosing an antibody that worked well, they tested it in mice and found the antibody had triggered conversion of Tregs to Teffs. The next step is to conduct a clinical trial using the approach in patients.25
T cells can also play a role in chemotherapy resistance in ovarian cancer patients. The tumor microenvironment is made up of many cell types, but the bulk tissue comprises effector T cells and fibroblasts. In a study at the University of Michigan, researchers looked at tissue samples from ovarian cancer patients and separated the cells by type to study the tumor microenvironment in vitro and in mice. They then linked their findings back to actual patient outcomes. Ovarian cancer is typically treated with cisplatin, a platinum-based chemotherapy. They found that fibroblasts block platinum, preventing it from accumulating in the tumor and destroying it. T cells, on the other hand, overruled the protection of fibroblasts. By adding the T cells to the fibroblasts, they found that tumor cells began to die off. And, by boosting the effector T cell numbers, the researchers were able to overcome the chemotherapy resistance in the mouse model. They also used interferon, an immune cell secreted cytokine, to manipulate the pathways involved in cisplatin. In essence, by re-educating the fibroblasts and tumor cells with immune T cells after chemo-resistance develops, the same chemotherapy can be used because it’s effective again.26
Another way of making cancer cells more sensitive to chemotherapy is with a fasting-like diet. Researchers at the University of Southern California found that a fast-mimicking diet, when used with chemotherapy drugs, raises the levels of bone marrow cells that generate immune system cells such as T cells, B cells and natural killer (NK) cells that infiltrate tumors. In their mouse study, the researchers also found that the T regulatory cells that protect cancer cells were expelled. They traced this effect to a weakened enzyme, heme oxygenase-1 or HO-1, inside the T regulatory cells’ mitochondria. HO-1 levels have been found to be elevated in tumors and are linked to several types of cancer.
The researchers examined the effects of a fast-mimicking diet on breast cancer and found that putting the mice on four days of the diet with chemo drugs doxorubicin and cyclophosphamide was as effective as two days of a water-only, short-term starvation diet. Both diets with the drugs slowed the growth of tumors while protecting healthy, normal cells. Similar effects were found with melanoma. They also found three cycles of the fasting diet combined with doxorubicin prompted a 33 percent increase in the levels of cancer-fighting white blood cells and doubled the number of progenitor cells in the bone marrow. The cancer-killing cells were also more effective at attacking and shrinking the tumors. In addition, the researchers found that short-term starvation and the low-calorie fasting-like diet in mice reduced the expression of the HO-1 gene in the T regulatory cells, making it easier for the chemotherapy drugs to attack the cancer.27
A new method of developing drugs that manipulates the immune system to fight cancer has also been developed by scientists at Rockefeller University’s Laboratory of Molecular Genetics and Immunology. Specifically, they developed a new mouse model to create drugs that target CD40, a protein present on certain immune cells that functions to activate them. To date, attempts to develop antibodies targeting CD40 have been disappointing.
The scientists started by creating mice whose immune systems more closely mimic those of people. The new mouse model expresses the human versions of both the CD40 protein and Fc receptors, a group of proteins expressed in immune cells that bind to the back side of antibody molecules in a region known as the Fc domain. They then looked for antibodies that bind them more tightly. They found that engagement of a certain human Fc receptor called FcRIIB is essential for the therapeutic activity of human CD40 antibodies, whereas engagement of a different receptor called FcRIIA compromises their activity. “We found from our study that current antibodies under development don’t fully utilize the potential of the CD40 approach,” said Rony Dahan, a postdoctoral fellow at the lab. “We have used our new model to identify and select new Fc-engineered CD40 antibodies that have significantly enhanced antitumor activity. We then advanced the most promising candidate into clinical trials of various solid tumor types.”28
Another method of using the body’s immune system to develop new immunotherapies that better fight cancer has been found by researchers at the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia. By switching off the protective measure that stops the body’s NK immune cells from attacking human tissue, they were able to drastically reduce tumor growth in mice. NK cells are specialized white blood cells that locate and kill deviant cells by releasing a chemical called perforin that blasts holes in its outer membrane and causes the cells to fall apart or self-destruct. But, the body’s immune system also possesses checkpoints to protect healthy tissue. The researchers discovered a particular checkpoint with an inhibitor protein made inside the cells that limited their ability to respond to the NK cells’ command to kill cancer.
In their study, they found that by silencing the inhibitor protein’s gene, the ability of NK cells to protect mice against melanoma, prostate cancer and breast cancer was increased. After 14 days, melanoma mice without the genetic modification had extensive tumor growth in their lungs. In contrast, metastatic growth was largely absent from mice with boosted NK cells. Mice with prostate cancer responded in a similar way. And, those with breast cancer showed that despite some microscopic spread to the lungs, there was no sign of the large metastases that would normally be observed. “This is about learning how to activate the NK cells of the individual patient and boost their immune system to tackle the disease,” said lead scientist Dr. Nicholas Huntington. “We are hopeful our research will lead to new immunotherapies that supercharge the body’s natural killer cells and maintain it in a highly active state to more efficiently and specifically fight cancer.”29
Another discovery by a team of researchers at the Duke Human Vaccine Institute and Duke medical faculty has resulted in the creation of a recombinant antibody, mAb7968, that can target the human protein complement factor H (CFH), which is abundant in tumor tissues and is believed to play a role in stifling an immunological response to malignant cancer cells. To develop the antibody, scientists examined early-stage tumors in lung cancer patients that never progress and noticed that, when compared with more lethal tumors, the patients possessed antibodies against CFH. After identifying the antibody for CFH, they extracted it from human tissue and modified it to enhance its function. The newly engineered antibody could induce toxic conditions in more than nine cancerous cell lines and, consequently, kill many of those cells without any noticeable side effects. “This could represent a whole new approach to treating cancer, and it’s exciting because the antibody selectively kills tumor cells, so we don’t have significant side effects to achieve tumor control,” said Edward Patz, Jr., professor at Duke University and senior author of the study. “We believe we can modulate the immune response and let the body’s own immune system take over to either kill the tumor or keep it from growing.”30,31
Lastly, researchers at the University of Eastern Finland and Eberhard Karls Universitat Tubingen in Germany have discovered a new molecular mechanism that can inhibit the growth of hepatocellular carcinoma, the most common liver cancer. Their study found that mouse and human liver cancer in which the function of the protein p53 is disturbed or inhibited is dependent on the interaction between the Aurora kinase A (AURKA) and MYC proteins. Using a specific drug molecule to interfere with the AURKA protein causes cancer cells to die. These findings, they say, can be used to develop treatments.32
Vaccines and Gene Therapy
Because cancer vaccines and gene therapy can sometimes interfere with the growth of specific cancer cells, they are often considered targeted therapies.
Preventive cancer vaccines have been available for some time, the first of which was approved in 1981. There are two types of cancer for which vaccines are approved: human papillomavirus and hepatitis B virus.33
Two cancer treatment vaccines are FDA-approved in the U.S. In April 2010, Provenge (sipuleucel-T, Dendreon) was approved for metastatic prostate cancer. Provenge stimulates an immune response to prostatic acid phosphatase, an antigen that is found on most prostate cancer cells. In clinical trials, it increased the survival of men with a certain type of metastatic prostate cancer by about four months. Unlike other cancer vaccines, which are only available in clinical trials, Provenge is customized to each patient. Then, in October 2015, FDA approved Imlygic (talimogene laherparepvec, Amgen) for the treatment of some patients with metastatic melanoma that cannot be surgically removed. Imlygic works by infecting or lysing cancer cells when injected directly into tumors, but it also induces responses in noninjected tumors.34
Cancer treatment vaccines work by boosting the body’s natural defenses to fight cancer. They’re designed to prevent cancer from coming back, destroy any cancer cells still in the body after treatment and stop a tumor from growing or spreading. But developing them is difficult for several reasons: 1) cancer cells suppress the immune system, which is how cancer is able to develop and grow (researchers are using adjuvants to try to fix this issue); 2) cancer cells develop from a person’s own healthy cells, which means cancer cells may not look harmful to the immune system, causing the immune system to ignore them; 3) larger or more advanced tumors are hard to get rid of using only a vaccine, which is why other treatments are used in conjunction; and 4) people who are sick or older can have weak immune systems, so their bodies may not be able to produce a strong immune response after vaccination.34
Despite these drawbacks, there are many vaccines currently being tested in clinical trials. One in particular has recently been shown to kill tumors and keep them from coming back. In development by Intensity Therapeutics, the INT230-6 vaccine is composed of two chemotherapy drugs that are injected into tumors to kick-start the immune system to fight back. In preclinical studies, “injection of INT230-6 into large colon cancer tumors in mice caused tumor shrinkage in 100 percent of the subjects, with up to 80 percent experiencing a complete response. Complete responders further experienced an immunologically based, durable vaccine-like effect that protected the animals from multiple re-inoculation challenges using the same colon cancer cell type.” According to Ian Walters, MD, of Intensity Therapeutics, “Even though we are using chemo, this works on the immune system. The tumors die from the inside out. When that happens, the immune cells can ‘see’ that it’s cancer and form an extremely powerful immune response. It’s almost a personalized vaccine.”35,36
Another cancer treatment vaccine that has been in development for more than 20 years is Morphogenesis’ ImmuneFx. It is an autologous cancer vaccine made from each patient’s own cancer cells that are typically collected at the time of surgery when the tumor is removed. While the vaccine is not approved for use in humans, a version of it called IFx-VET is approved by FDA for use in animals, mostly in dogs and horses.37 In fact, at the Cancer Moonshot summit held at Howard University in Washington, D.C., in June, a golden retriever diagnosed with melanoma in her mouth attended as an example of the vaccine’s success in conjunction with radiation.38
Ultimately, what could be most promising is a “universal” cancer vaccine, which is also a type of personalized gene therapy that is being actively pursued. Researchers from Johannes Gutenberg University have developed a potential universal cancer vaccine based on the immune system’s natural responses to viral infection. In early experiments in mice and three human patients with advanced melanoma, the vaccine, which consists of nanoscale poison darts with RNA payloads, was able to induce specific anti-tumor immune responses. RNA darts introduce genetic material that mimics a virus. In response, dendritic cells produce cancer-specific antigens that prompt a T-cell response directed against progressive tumors — those that otherwise would be treated as normal by the immune system. According to professor Ugur Sahin, who is lead scientist in the study, “Virtually any tumor antigen (protein) can be encoded by RNA. Thus, the nanoparticulate RNA immunotherapy approach introduced here may be regarded as a universally applicable novel vaccine class for cancer immunotherapy.”39,40
Another promising gene therapy tool may be tested in humans in the very near future. Known as CRISPR, the gene-editing tool that rewrites immune system DNA, has won approval to proceed with its first human tests from the Recombinant DNA Advisory Committee, a federal ethics panel at the National Institutes of Health that reviews controversial experiments that change the human genome (the trial still needs final approval from FDA). Scientists from the University of Pennsylvania want to use CRISPR to edit the immune systems of 18 patients to target difficult-to-treat cases of multiple myeloma, sarcoma and melanoma. If the trial proceeds, the scientists will remove blood samples from patients, alter their T cells and then infuse them back into patients to evaluate the safety and effectiveness of the technique.41
Several Phase III gene therapy clinical trials that hold promise are also currently underway, including:
- Advantagene is using Gene Mediated Cytotoxic Immunotherapy (GMCI) ProstAtak therapy, which uses an adenovirus vector to deliver a herpes simplex virus thymidine kinase (tk) gene to tumor cells at the site of the injection. The tk gene works as a “suicide gene” that enzymatically converts a nontoxic, antiviral drug Valacyclovir into a cytotoxic drug that causes tumor cell death during radiotherapy.
- VBL Therapeutics is using its Vascular Targeting System known as VB-111 to treat recurrent glioblastoma multiforme. The gene therapy targets a highly malignant type of angiogenic brain tumor that generates vasculature tissue in a process known as angiogenesis. It is intended to be used in combination with chemotherapy and radiotherapy.
- Cold Genesys’ adenovirus-mediated oncolytic gene therapy is targeting invasive bladder cancer. Similar to T-Vec, the CG0070-modified virus contains a cancer-specific promotor sequence and GM-CSF-encoding sequence that selectively lyses cancer cells and releases GM-CSF antigen to train the immune system.42
Targeting Drugs to Patients
With so many cancer treatments on the horizon, an additional problem still exists: No two cancers are the same, which means no two cancer patients respond the same to medication. Therefore, to prescribe the correct combination and dosage of drugs, physicians need a better understanding of the specific characteristics of each patient’s cancer.
Enter CANScript, Mitra Biotech’s promising technology that can rapidly test the impact of drugs on a cancer patient by examining a tiny tumor sample in a lab. Removed during a biopsy, the tumor tissue is tested with multiple drugs to replicate a patient’s reaction to the medications. CANScript measures a number of parameters, including tumor cell death, cell shape and structure and rate of tumor growth, to assign a single numeric score to a particular drug or combination of drugs. The higher the score, the greater the chance of tumor burden reduction.
In a study of CANScript conducted in 2015, the microenvironment of 109 patients suffering from head and neck squamous cell carcinoma and colorectal cancer was recreated. Researchers then tested the response of a set of drugs on the tumors, from which data were used to shape a predictive model. The model was then tested on a group of 55 patients with one of the cancers and treated with the same drugs. In the test, CANScript correctly predicted each cancer patient’s response to the treatment.
CANScript delivers results with seven days at a cost of approximately $600.43
Declaring War on Cancer
Clearly, revolutionary advances are being made in the war on cancer. According to Vice President Joe Biden, who is spearheading the Obama administration’s “moonshot” to cure cancer, the science is ready. “But the science, data and research results are trapped in silos, preventing faster progress and greater reach to patients. It’s not just about developing game-changing treatments; it’s about delivering them to those who need them,” explains Biden. “Right now, only 5 percent of cancer patients in the U.S. end up in a clinical trial. Most aren’t given access to their own data. At the same time, community oncologists — who treat more than 75 percent of cancer patients — have more limited access to cutting-edge research and advances.” Biden’s task, then, is to increase public and private resources to fight cancer and bring together researchers, philanthropists, Big Pharma and insurers. The federal effort will also fund research into how different immunotherapy treatments work in combination with one another, as well as efforts to improve prevention and early detection. However, says Massachusetts Institute of Technology cancer researcher Robert Weinberg: “The war on cancer will not be won in one dramatic battle. It will be a series of skirmishes.”44
References
- National Cancer Institute. Surveillance, Epidemiology and End Results Program Stat Fact Sheets:Cancer of Any Site. Accessed at seer.cancer.gov/statfacts/html/all.html.
- IMS Health Study: Global Market for Cancer Treatments Grows to $107 Billion in 2015, Fueled by Record Level of Innovation. Accessed at www.imshealth.com/en/about-us/news/ims-health-study-global-market-for-cancertreatments-grows-to-107-billion-in-2015-fueled-by-record-level-of-innovation.
- Fayed, L.The History of Cancer. VeryWell, June 2, 2014. Accessed at www.verywell.com/the-history-of-cancer-514101.
- Evan, G. Expert Opinion: Why Are Some Cancers So Difficult to Treat? Cancer Research UK, Jan. 26, 2012. Accessed at scienceblog.cancerresearchuk.org/2012/01/26/expert-opinion-why-are-some-cancers-so-difficult-to-treat.
- Walker, J. A&M Researchers Make Cancer Discovery About How Cells Escape Past Immune System. TheEagle.com, May 10, 2016. Accessed at www.theeagle.com/news/a_m/a-m-researchers-make-cancer-discovery-about-howcells-escape/article_d262844e-166d-11e6-b693-8fec3b5fecc7.html.
- Structural Variant in PD-L1 Regulatory Region Helps Some Cancers Dodge Immune System. Genome Web, May 23, 2016. Accessed at www.genomeweb.com/sequencing/structural-variant-pd-l1-regulatory-region-helps-somecancers-dodge-immune-system.
- Novel Insights Into Metastasis Could Offer New Treatments. The Medical Frontier, June 25, 2016. Accessed at www.themedicalfrontier.com/2016/06/novel-insight-metastasis-offer-new-treatments-2.
- McGinley, L. Here Are Some Ways Cancer Can Thwart the New Immunotherapy Drugs. The Washington Post, July 13, 2016. Accessed at www.washingtonpost.com/news/to-your-health/wp/2016/07/13/here-are-some-ways-cancer-can-thwart-the-new-immunotherapy-drugs.
- National Cancer Institute. Targeted Cancer Therapies. Accessed at www.cancer.gov/about-cancer/treatment/types/targeted-therapies/targeted-therapies-fact-sheet.
- My Cancer Genome. Overview of Targeted Therapies for Cancer. Accessed at www.mycancergenome.org/content/molecular-medicine/overview-of-targeted-therapies-for-cancer.
- Vanneman, M and Dranoff, G. Combining Immunotherapy and Targeted Therapies in Cancer Treatment. Nature Reviews, 12, 237-251 (April 2012). Accessed at www.nature.com/nrc/journal/v12/n4/full/nrc3237.html.
- Loftus, P. New Hope for Melanoma Patients — Update. Dow Jones Business News, May 18, 2016. Accessed at www.nasdaq.com/article/new-hope-for-melanoma-patients–update-20160518-01315.
- Kennelty, G. Understanding the Future of Immunotherapy in Melanoma. Targeted Oncology, May 9, 2016. Accessed at www.targetedonc.com/news/understanding-the-future-of-immunotherapy-in-melanoma.
- Nivolumab Immunotherapy Helps Patients with Advanced Bladder Cancer. Science Daily, June 5, 2016. Accessed at www.sciencedaily.com/releases/2016/06/160605124112.htm.
- Fox, M. New Immune Therapy Drug Gives BladderCancer Patients Fresh Hope. NBCNews, June 5, 2016. Accessed at www.nbcnews.com/health/cancer/new-immune-therapy-drug-gives-bladder-cancer-patients-fresh-hope-n585606.
- Tiller, E. Experimental Therapy Based on Immune-System Antibodies May Help Stomach Cancer Patients. MyInforms.com, June 6, 2016. Accessed at myinforms.com/en-us/a/35582717-experimental-therapy-based-on-immune-system-antibodies-may-help-stomach-cancer-patients.
- Semedo, D. New Brain Cancer Treatment Study Is Immunotherapy-Based. Immuno-Oncology News, May 19, 2016. Accessed at immuno-oncologynews.com/2016/05/19/national-brain-tumor-society-oligo-nation-announce-funding-immunotherapy-based-approach-oligodendroglioma-treatment.
- Tate, N. Can the Polio Virus Cure Cancer? NewsMax, March 30, 2015. Accessed at www.newsmax.com/ Health/Health-News/polio-virus-cancer-cure/2015/03/30/id/635309.
- FDA Fast-Tracks Treatment That Uses Polio Virus to Fight Brain Cancer. Fox News, May 13, 2016. Accessed at www.foxnews.com/health/2016/05/13/fda-gives-approval-to-using-polio-to-fight-terminal-brain-cancer.html.
- Chiu, E. UCLA Researchers Develop New Immunotherapy for Advanced Brain Cancer. Daily Bruin, July 18, 2016. Accessed at dailybruin.com/2016/07/10/ucla-researchers-develop-new-immunotherapy-for-advanced-brain-cancer.
- Cristol, H. FDA Approves Opdivo for Hard-to-Treat Hodgkin Lymphoma. American Cancer Society, May 18, 2016. Accessed at www.cancer.org/cancer/news/news/fda-approves-opdivo-for-hard-to-treat-hodgkin-lymphoma.
- Novel Immunotherapy Trial for Lymphoma Offers Hope to Patients. MedicalXpress, May 24, 2016. Accessed at medicalxpress.com/news/2016-05-immunotherapy-trial-lymphoma-patients.html.
- Berkrot, B. Pfizer Cancer Drug Shows Promise in Combo with Merck’s Keytruda. Reuters, May 18, 2016. Accessed at www.reuters.com/article/us-health-cancer-pfizer-immunotherapy-idUSKCN0Y92W2.
- Radiation and Immunotherapy Combination Can Destroy Both Primary and Secondary Tumors. Science Daily, May 1, 2016. Accessed at www.sciencedaily.com/releases/2016/05/160501142559.htm.
- New Cancer Immunotherapy Approach Combines Tumor Fighting Power with Fewer Side Effects. Science Daily, May 16, 2016. Accessed at www.sciencedaily.com/releases/2016/05/160516151926.htm.
- T Cells Help Reverse Ovarian Cancer Drug Resistance. Genetic Engineering and Biotechnology News, May 23, 2016. Accessed at www.genengnews.com/gen-news-highlights/t-cells-help-reverse-ovarian-cancer-drug-resistance/81252753.
- Gersema, E. Fasting-Like Diet Turns the Immune System Against Cancer. USC News, July 12, 2016. Accessed at news.usc.edu/103972/fasting-like-diet-turns-the-immune-system-against-cancer.
- New Mouse Model Gives a Boost to the Development of Cancer Immunotherapies. Science Daily, June 2, 2016. Accessed at www.sciencedaily.com/releases/2016/06/160602151856.htm.
- Tamblyn, T. Scientists Discover Hidden Switch in Our Immune System for Fighting Cancer. Huffington Post, May 24, 2016. Accessed at www.huffingtonpost.co.uk/entry/scientists-discover-hidden-switch-in-our-immune-system-for-fighting-cancer_uk_57442732e4b0e71ef36da559.
- MacDonald, T. Scientists Discover Human-Derived Antibody that Targets, Destroys Cancer Cells. MyInforms.com, May 5, 2016. Accessed at myinforms.com/en-us/a/32620777-scientists-discover-human-derived-antibody-thattargets-destroys-cancer-cells.
- Patel, V. Duke Researchers Develop Antibody Able to Target Cancerous Tumors. The Chronicle, June 7, 2016. Accessed at www.dukechronicle.com/article/2016/06/duke-researchers-develop-antibody-able-to-target-cancerous-tumors.
- Dauch, D, Rudalska, R, Cossa, G, et al. A Protein Complex Represents an Actionable Drug Target in p53-Altered Liver Cancer. Nature Medicine (2016), published online May 23, 2015. Accessed at www.ncbi.nlm.nih.gov/pubmed/27213815.
- National Cancer Institute. Cancer Vaccines. Accessed at www.cancer.gov/about-cancer/causes-prevention/vaccines-fact-sheet.
- Cancer.Net. What Are Cancer Vaccines? Accessed at www.cancer.net/navigating-cancer-care/how-cancer-treated/immunotherapy-and-vaccines/what-are-cancer-vaccines.
- Adams, S. Vaccine Breakthrough May Cure Cancer and Stop It Returning. Daily Mail, May 7, 2016. Accessed at www.dailymail.co.uk/news/article-3577432/Vaccine-breakthrough-cure-cancer-stop-returning.html.
- IntensityTherapeutics,Inc. Reports Anti-Cancer Immunological Effect Generated By INT230-6. BioSpace, March 3, 2016. Accessed at www.biospace.com/News/intensity-therapeutics-inc-reports-anti-cancer/411048.
- Morphogenesis. IFx-VET Cancer Vaccine. Accessed at www.morphogenesis-inc.com/veterinary-oncology/veterinarians.
- Cancer Vaccine Helps Tampa Dog with Melanoma, Raising Hope for Humans. Fox News, June 30, 2016. Accessed at latino.foxnews.com/latino/health/2016/06/30/cancer-vaccine-helps-tampa-dog-with-melanoma-raising-hope-for-humans.
- Lerche, O. A Tumor Vaccine Which Tricks the Immune System Could ‘Treat’ All Cancers, Say Experts. Express, June 2, 2016. Accessed at www.express.co.uk/life-style/health/676078/tumour-vaccine-which-tricks-the-immune-system-treat-all-cancers.
- Byrne, M. A Universal Cancer Vaccine Might Be Closer Than You Think. Motherboard, June 1, 2016. Accessed at motherboard.vice.com/read/a-universal-cancer-vaccine-immune-defenses-rna.
- Randall, T. Crispr Wins Key Approval to Fight Cancer in Human Trials. Bloomberg Technology, June 23, 2016. Accessed at www.bloomberg.com/news/articles/2016-06-23/crispr-wins-key-approval-to-fight-cancer-in-human-trials.
- Personalized Gene Therapy to Fight Against Cancer. NewsMedical, March 25, 2015. Accessed at www.newsmedical.net/news/20150325/Personalized-gene-therapy-to-fight-against-cancer.aspx.
- Ghoshal, D. In Just Seven Days, This Indian Biotech Firm Can Tell Cancer Patients the Ideal Course for Their Treatment. Yahoo Finance, Sept. 20, 2016. Accessed at finance.yahoo.com/news/just-seven-days-indianbiotech-063626614.html.
- The New War on Cancer. The Week, May 15, 2016. Accessed at theweek.com/articles/623940/new-war-cancer.