PTSD: A Patient’s Perspective
According to the National Institutes of Health, approximately 7.7 million American adults age 18 and older suffer symptoms of post-traumatic stress disorder (PTSD). Thankfully, emerging treatments are providing relief and recovery, even in the most severe cases.
- By Trudie Mitschang
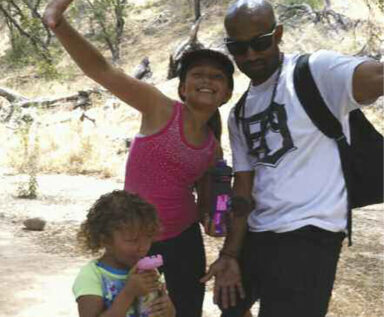
DELON BECKETT IS a soft-spoken, thoughtful man, with an easy sense of humor and a quick smile. But, less than a year ago, the married father of two was withdrawn, angry and suicidal. The Iraq War veteran was suffering from undiagnosed post-traumatic stress, and his life was slowly unraveling.
An Iraq War Veteran
Beckett began his tour of duty in August 2010, and although the 28-year-old did not see active combat, living under the constant barrage of mortar shells took an intense toll on his psyche. “When I went home on my first leave, something snapped. I was not excited to see my family, I was anxious and angry,” he recalls. “When I returned, my platoon sergeant noticed a change in me and sent me to talk to one of the combat doctors.”
Beckett was put on anti-depressants and anti-anxiety medication, and when his tour of duty ended, he was sent to a treatment center in Fort Irwin, Calif., for psychological evaluation. But, within two months, he was abruptly discharged and labeled “the VA’s problem.” “I had to wait a month to get into the VA program, and I had no access to my medications,” he says. “That’s when I started drinking, to cope with the withdrawal symptoms.”
Beckett eventually began treatment through the VA and was prescribed a plethora of medications, including mirtazapine, bupropion and clonazepam (Klonopin) to address his depression, anxiety and sleep disorders. He also began seeing a counselor. But it was not until March 2014 that he faced the fact that he needed additional help. “The medications masked all my emotions so that all I could feel was rage,” he explains “I was very withdrawn and could not handle more than a five-minute conversation with my wife. When I got word that one of my friends from my platoon had committed suicide, I hit rock bottom and wanted to kill myself too. That’s when a mental health specialist employed by the VA told me about the Save a Warrior Program (SAW).”
Swapping Medication for Meditation
Started by veteran Jake Clark, the SAW program is an intensive five-day “war detox” for veterans suffering from PTSD. Featured in the CNN documentary “The War Comes Home,” SAW combines an unconventional mix of equine therapy, transcendental meditation and trust-building exercises to help traumatized soldiers heal. Hosted at the scenic Big Heart Ranch in Malibu, Calif., the program has been extremely successful in providing a non-pharmaceutical model for helping traumatized veterans. The $1,200 cost of the program, which includes dormitory accommodations, is completely covered by corporate and other donations.
For Beckett (whose story is featured in the documentary), the program was transformative. He says he learned about the childhood issues that predisposed him to PTSD, and has been able to take responsibility for how his behavior has impacted his family. “It really is amazing what a horse can do for you!” he laughs. “The transcendental meditation was also incredibly impactful; since completing the program, I now meditate daily, and I believe it has kept me sober. I have not touched a drink since finishing the SAW program.” Beckett is still in touch with his buddies, the veterans who completed the program with him, and he says the accountability and camaraderie have been a lifeline for him. He is completely off medications, continuing in family counseling, and for the first time in a very long time, optimistic about the future. “The SAW program put me on a path of self-discovery. Now I feel empowered to write my own story and pursue a career path that includes helping others,” he says. “I don’t have to live paranoid or self-conscious — I’m not scared anymore.”