Addressing Central Pain Syndrome
Central pain syndrome affects several million people worldwide, yet this condition wasn’t fully understood until recently, and there are still many challenges concerning diagnosis and treatment.
- By BSTQ Staff
JUST A FEW years ago, Radene Marie Cook was busy balancing demanding careers. She was a professional actor, dancer and singer. She was also a popular on-air personality whose resume includes being an “On the Spot” news and airborne traffic reporter for KFWB in Los Angeles, Calif. But Cook’s life changed when, while on assignment, her plane was involved in an accident after being hit by a microburst. “The midair collision with the winds moving straight down at nearly 200 miles per hour was like the force of an 18-wheeler slamming into a Soap Box Derby car,” she says.1
Cook sustained serious injuries to her head and back, but that wasn’t the worst of it. Her workers’ compensation program required her to have a discogram as part of her rehabilitation. This invasive procedure is designed to help physicians determine the anatomical source of a patient’s back pain. During a discogram, dye is injected into the center of one or more spinal discs to pinpoint which ones are causing pain. The injection can reproduce back pain in the affected disc or discs. The dye also makes cracks in the exterior of discs visible on an X-ray or CT scan.2
The procedure is controversial in part because it’s not always effective and in part because of potential complications.2 In Cook’s case, the needle punctured her spinal cord lining, which resulted in adhesive arachnoiditis, a condition characterized by complete encapsulation of the nerve roots. Adhesive arachnoiditis has been described as a life sentence of unremitting pain,3 and Cook wasn’t spared that outcome. After the discogram, her central pain syndrome symptoms appeared. As time passed without a proper diagnosis or treatment, her symptoms proliferated and also increased in severity. “The longer the pain went undertreated, the worse my overall health got,” she says. “First, the symptoms themselves got more severe. Then, there were more of them.”
Cook says it took three years before she was diagnosed with central pain syndrome and numerous associated conditions. Along the way, she received several misdiagnoses and encountered physicians who told her they had no idea what was going on. In her words, they “just threw up their hands.” The correct diagnosis came from a neurologist in Alabama who specializes in detecting difficult-to-diagnose spinal issues.
What Is Central Pain Syndrome?
First described in 1891, central-type pain was believed to be caused by stroke-related damage of the thalamus. 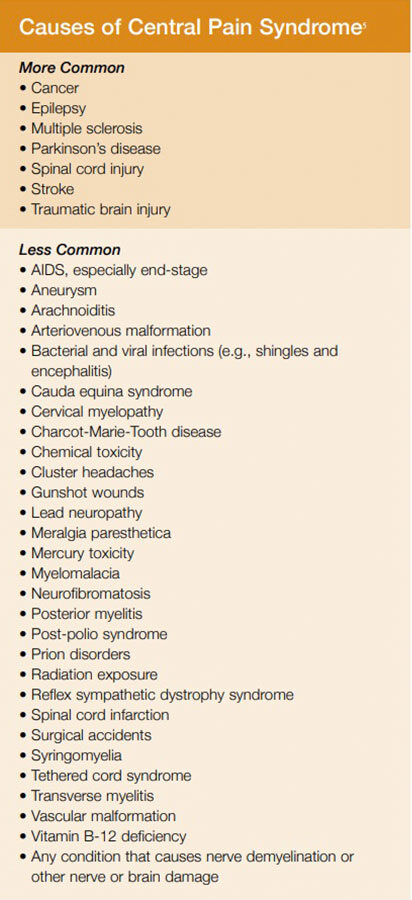 It was later believed to be caused by a thalamic syndrome that included a pain component. Until recently, thalamic pain was the prevailing understanding of central pain.4,5
It was later believed to be caused by a thalamic syndrome that included a pain component. Until recently, thalamic pain was the prevailing understanding of central pain.4,5
According to the National Organization for Rare Disorders, researchers now understand that damage to the pain-conducting pathways anywhere along the neural axis, from the spinal cord to the sensory cortex, can cause central pain syndrome, which can be broken down into central pain of brain or brain stem origin or central pain of spinal cord origin.4 The term “central pain syndrome” reflects the fact that damage to various areas of the central nervous system (CNS) can cause central pain and that a stroke is not necessarily the primary cause. Brain or spinal cord trauma, epilepsy, multiple sclerosis, Parkinson’s disease and tumors can also cause central pain syndrome. 6 (See Causes of Central Pain Syndrome for additional causes.)
Sarah Dominguez, a specialty physical therapist who treats central pain syndrome and owner of Foundational Concepts in Kansas City, Mo., says central pain syndrome is different from chronic pain since it’s caused by an insult to the CNS rather than pain that develops over time from an old injury such as one to the back or knee. “The pain originates from the CNS, not from the nerves in the periphery. It is similar to chronic pain as they both cause changes to the CNS, making the brain and nerves more sensitive to movement, thus enhancing the pain experience,” she explains.
Because there are a variety of causes, the syndrome differs from person to person. Some experience pain over a large portion of the body, while others may have pain in a specific area. Though each person is different, the pain is typically constant and moderate to severe. Touch, movement, emotions, temperature changes and other factors can affect the level of pain.6 The type of pain may be aching, burning, freezing, lacerating, pressing, shocking or tearing in nature — or what can best be described as pins and needles. Brief bursts of sharp pain can also occur, as can numbness in the areas affected by the pain.5,6 Central pain syndrome often begins shortly after the injury or damage occurs, but months or even years can pass before the pain starts, according to the Central Pain Foundation.6
Along with intense, unrelenting, multifaceted pain, Cook experienced pain in parts of her body that had not been injured, hyperhidrosis and hypothalamus dysfunction, and allodynia (central pain sensitization following painful, often repetitive, stimulation). “I had sharp, electric, lancinating-type pain anywhere and everywhere — my legs, my sides, my arms, everywhere, especially in bizarre places like the one that would wake me up in the middle of the night: the sides of my tongue,” she says. “It would feel like someone had attached a jumper cable to the middle of my tongue, then hooked that jumper cable to the nearest electric chair.”
The allodynia affected her from head to toe. The hyperhidrosis made her sweat in strange patterns. The hypothalamus dysfunction made her feel nauseated at 85 degrees and led her to pass out at temperatures higher than 98 degrees. “Honestly, you could mix the electric chair pain with invisible knife wounds and throbbing pressure, and you pretty much have the pain range I am describing,” she says. In fact, Cook’s pain is so severe that she has to lie on a mattress in the back of a van when traveling to and from doctor appointments. Sitting for long distances is out of the question.
A Difficult Diagnosis
Dominguez says a major impediment to early diagnosis and treatment is that symptoms can lag behind injury for years. Healthcare providers are traditionally trained to treat acute onset of pain or symptoms, not delayed symptoms. In addition, there are no ideal diagnostic tests to detect CNS hypersensitivity, which further inhibits diagnosis.
Beyond that, the system itself can hamper diagnosis, she says. She describes one scenario for illustration: Patient X begins having burning pain in his hands. He goes to his primary doctor, who prescribes some sort of pain medication and refers him to a specialist. It takes two to three months to get an appointment, giving Patient X’s CNS more time to continue forming bad habits regarding sensitivity. The specialist needs tests and procedures. This takes more time. Meanwhile, Patient X’s feet are now burning along with his hands, and his brain is racing to solve this pain puzzle by itself. This causes anxiety, worry and fear, which only increase pain sensitivity in the CNS. The procedures finally come, but show nothing, so Patient X is referred to another specialist (e.g., neurology, rheumatology, orthopedic), which takes another month or two, and the cycle continues until Patient X has spent three years just getting to a diagnosis.
This all-too-common scenario is very similar to the one Cook experienced on her own three-year quest for medical answers and appropriate treatment.
Dominguez adds that, while knowledge about central pain syndrome has been building over the past decade, clinical practice often lags behind research: “Many therapists simply have not learned how to best approach these types of patients. Our role as a physical therapist (PT) is to educate our patients about pain physiology, utilize our knowledge of the nervous and musculoskeletal systems, and work with movement to restore function.” She adds that a PT’s job is to avoid setting unachievable goals. The goal isn’t to make people with chronic pain pain-free, she says, because that’s not realistic. Instead, the focus is on function, recreation and quality of life — elements all healthcare providers can focus on with regard to the care they provide.
Lynn R. Webster, past president of the American Academy of Pain Medicine, echoes Dominguez’s statement about avoiding the goal of making patients pain-free: “Clinicians should assess and treat underlying disorders that cause pain, and they should work to eliminate the pain, but they should also understand that, for some patients with some types of pain, eradicating all underlying causes or the pain itself may not be possible.”
Why Treatment Matters
Webster says that, despite the inability to remove all causes of pain in all patients, pain must be addressed and prioritized.7 To do otherwise, he says, is to “put patients at risk for a host of complications, the most serious of which is the progression to pain as a chronic destructive pathology.”
In an effort to prevent chronic pain from developing in the first place, Webster says pain should be assessed in patients as frequently as vital signs are assessed. Unfortunately, some providers don’t quite know what to do with pain, including central pain syndrome, when it does present in a patient. This stems in part, says Dominguez, because central pain syndrome is hard to see, difficult to reproduce and a challenge to treat. Others might be reluctant to treat complex forms of pain because opioid addiction is on the rise. Some healthcare providers assume opioids are the only way to treat chronic pain, and they don’t want to manage that class of medications. They might even think patients with central pain are drug-seeking or have emotional or mental health issues that are causing their pain.5 Yet, delays in treatment because of these misperceptions only make central pain syndrome worse.
Cook’s current therapy is high-dose opioids along with several supplements to help her body fight the constant onslaught of pain. This regimen has allowed her to live in a way that’s plugged in — not checked out — to her creativity, to her spirit and to her purpose.
According to Dominguez, the appropriate treatment matters a great deal, especially from the standpoint of physical therapy. “The current research shows that when we educate patients about the physiology of pain, they feel better. Why? Because when they have a better understanding of their pain, the brain calms down, stops worrying and does not fear what it does not know,” she says. She also says it’s important for healthcare providers to develop a team approach to central pain syndrome: “One provider alone will not have all the answers. A physician who understands the condition, a mental health provider, physical therapy and often many alternative therapies are important parts of the team.”
A Healing Journey
Pain patients aren’t lost causes. Their pain can be addressed, and they can learn to live with it, not in spite of it. Take Cook, for example. These days, she’s touching people’s lives in a new way. The former actor and news reporter spends her time working as an advocate for people who suffer from chronic pain. Along with other outreach work, she has put a face to pain through the INvisible Project, a program of the U.S. Pain Foundation that uses portraits of people living with chronic pain to educate others about these complex conditions. “Although I am still in pain, my life is improving significantly,” her profile states. “It is because I have access to the opioid treatment appropriate for me, and because of the individualized treatment plan worked out between me and my doctor, that I can again have a quality of life that overshadows the pain — something I could not have when left to ‘fail-first’ treatment plans.”1

Her words say it all. Appropriate diagnosis and treatment, a patient-centered plan of care and the understanding that there’s no quick fix are essential when treating people with central pain. Within this framework, healthcare providers can come alongside their patients — and stay beside them — as they reclaim their health and their lives.
References
- INvisible Project. Radene Marie Cook. Accessed at www.invisibleproject.org/www/participants/2013-participants/radene-marie-cook.
- Mayo Clinic. Tests and Procedures: Discogram. Accessed at www.mayoclinic.org/tests-procedures/discogram/basics/definition/prc-20013848.
- Andreae-Jones S. Adhesive Arachnoiditis: A Continuing Challenge. Practical Pain Management, March 1, 2004. Accessed at www.practicalpainmanagement.com/pain/spine/adhesive-arachnoiditisa-continuing-challenge.
- National Organization for Rare Disorders. Central Pain Syndrome. Accessed at rarediseases.org/rare-diseases/central-pain-syndrome.
- Central Pain Foundation. Information for Medical Providers. Accessed at centralpainsyndromefoundation.com.
- National Institute of Neurological Disorders and Stroke. Central Pain Syndrome Information Page. Accessed at www.ninds.nih.gov/disorders/all-disorders/central-pain-syndrome-information-page.
- Webster LR. Yes, Assessing Pain Is Vital. Pain Medicine News, June 20, 1016. Accessed at www.painmedicinenews.com/Commentary/Article/07-16/Yes-Assessing-Pain-Is-Vital/36824.