Avoiding Part B Reimbursement Pitfalls
- By Bonnie Kirschenbaum, MS, FASHP, FCSHP
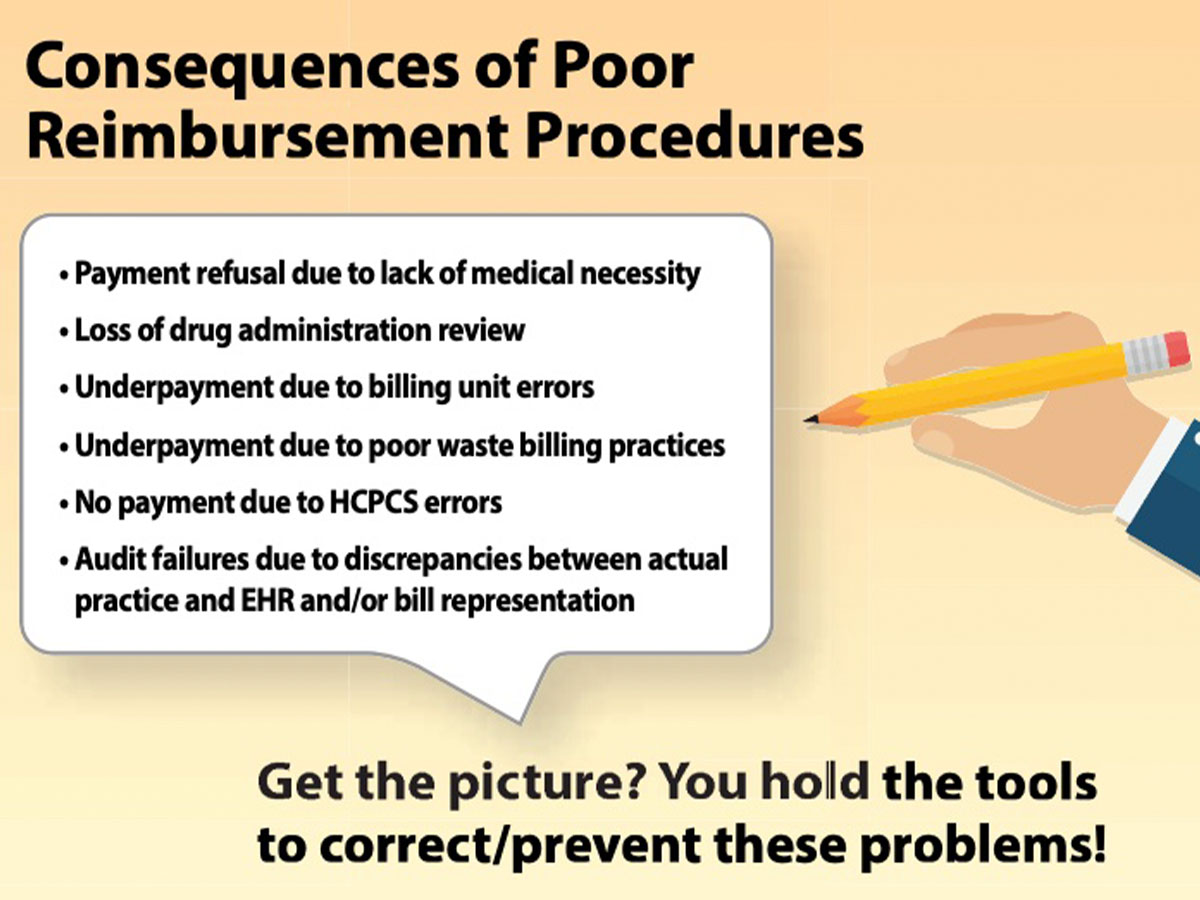
AS HEALTHCARE PRICES continue to skyrocket, practitioners can help to mitigate the impact by fully meeting the reimbursement requirements for Part B drugs in outpatient settings. Providing all appropriate information for reimbursement ensures payment is forthcoming when a patient’s story is told completely and accurately in a codeable fashion that describes what was done and what was used.
Review Documentation for Reimbursement
First, be sure the diagnosis that supports the drug use is charted completely for detailed ICD-10 assignment by the revenue cycle team. Next, verify the name of the drug is linked to a Healthcare Procedural Coding System (HCPCS) code. If a miscellaneous HCPCS code is used in the interim before permanent assignment, the national coverage determination (NCD) number must accompany it as well. Payment is for the actual dose of the drug administered, not for the amount of the drug in a vial or package. This actual dose is converted into billing units using the Centers for Medicare and Medicaid Services (CMS)-created values. The amount of drug waste, if applicable, is also converted into billing units and assigned the JW modifier. The CMS-assigned status indicator (SI) determines the payment classification. If the drug has been given by an intravenous (IV) infusion, then electronic health record (EHR) documentation supporting an injectable drug administration charge is essential.
Who, What and Why?
Where does all this information come from, and who is responsible for providing it? The diagnosis that supports the choice of the drug and its use is essential, and it must be documented completely and accurately in the EHR by the clinician ordering the drug. The use of a computerized physician order entry (CPOE) should support the requirements outlined in prior authorization (PA) requirements set by the payer and the local/national coverage determination (LCD/NCD) requirements set by Medicare.
How this is done and who is responsible for creating the appropriate order sets depends on core competency. Similarly, core competency is necessary for the correct assignment of the HCPCS code and the creation of the billing unit conversion crosswalk. Commercial resources may be available at the practitioner’s site. If so, they should be used to their maximum potential. This also applies to recovering revenue for waste. Never assume the initial assignment is error-free. It must be checked and rechecked at each step of the transmission throughout the revenue cycle process. The SI assigned to the drug will signal what revenue to expect and the method of payment, either separate or bundled. Most expensive products used in the outpatient prospective payment system (OPPS) setting are given by IV infusion, which is reimbursed separately from the drug itself. EHR documentation supporting this charge is essential, so it should be incorporated into the EHR system to ensure the process is seamless and accurate with an automatic prompt for documentation of administration.
Examples of Documentation Gone Wrong
Examples of inappropriate paths a drug can take may provide some ideas of where problems could be encountered and how to correct them to ensure payment.
Example: A patient is registered appropriately, including payer information, but the payer information is not passed on to the pharmacy. Or, the prescriber charts scantily because he/she is not aware of what is necessary, and the revenue cycle team assigns codes that don’t meet payer requirements.
Correction: Make payer information automatically available to the pharmacy. The CPOE file system should include PA/LCD/NCD information so payer requirements are available at the time of drug order entry. If this is not done, neither the prescriber nor the pharmacy is aware of the requirements.
Example: A place was not created in the EHR for the details of the PA to be documented.
Correction: The EHR should be retooled to accommodate payment requirements. To do otherwise risks claim denial due to lack of medical necessity. It’s not that the drug choice is wrong or the patient does not meet the criteria for its use. Payment refusal was due to a cascade of poor choices and actions by the clinical and IT teams in setting up the EHRs.
Example: A mismatch occurred between the pharmacy drug master (PDM)/charge description master (CDM) and the HCPCS billing units and SI.
Correction: Vigilance is essential with these two dynamic file sets. Regular review of the progression of charges through the various IT systems is necessary to identify glitches. It’s unacceptable to follow a “set it, forget it and don’t routinely check it” procedure.
Example: The pharmacy is unaware of how to bill for wasted payable injectable drugs from single-dose vials, amps and syringes.
Correction: Create a candidate list by identifying SI G- and K-eligible drugs, and update it quarterly. Billing unit conversions are essential for waste, as well as for the actual dose of the drug used. This can only be accomplished if an accurate crosswalk with the PDM/CDM is set up to accommodate required charting. Also, the pharmacy must continually follow up on this. It cannot opt for “robo-billing” in which the revenue cycle team has no idea what the clinician or IV preparation area actually did, but simply churned out bills based on an IT infrastructure. The ultimate test of success is a match between the actions of a clinician or IV prep area and what is actually charted and billed.
Example: A pharmacy is unaware of how to implement the 2018 OPPS 340B reimbursement changes, and it either overestimated or underestimated the financial impact.
Correction: Identifying the candidate drugs is an essential first step with the creation of a list of eligible SI K drugs purchased at 340B price that is updated quarterly. Modifier assignment is a CMS requirement. An accurate crosswalk must be provided to the revenue cycle team of SI K drugs bought at 340B price requiring the JG modifier and SI G drugs bought at 340B price requiring the TB modifier. Once again, reality must match billing. All 340B drugs must be accurately represented with the JG modifier on Medicare bills only for 340B-eligible patients.
A Shared Responsibility
As practices move forward, they must stay alert to changes and recognize everyone shares the responsibility for reimbursement. No one person has all the core competencies needed. Reimbursement can only be successful through teamwork and designating who is going to do what. This means the pharmacy and therapeutics committee makes wise progressive decisions, clinicians write complete orders, IT creates a favorable system, pharmacy, nursing and social services do their parts, and the revenue cycle team submits the code sets that tell the patient’s story completely and accurately.