Foodborne Illness: A Continuing Threat to Public Health
With more than 250 foodborne illnesses identified, it is often difficult to diagnose when a person has been infected to ensure proper treatment is prescribed.
- By Jim Trageser
Amid-20th-century doctor looking back at his own career recalled that, during his medical training in the early 1900s, he and other students were called over to a specific cadaver by the training physician. They were told that they should take a look at the lung cancer in the donated body because they might not ever see another case in their careers, whereas they could expect to see hundreds of cases of stomach cancer, at the time one of the most common types of malignancies. Of course, the introduction and marketing of pre-rolled cigarettes led to a stunning increase in lung cancer rates, while stomach cancer rates have plummeted in the United States and other developed nations thanks to the widespread adoption of refrigeration1 (made possible due to the development of dependable electricity supplies) and food safety practices.
If stomach cancer is not as rare today as lung cancer was in the 19th century, its radically lower rate is nevertheless emblematic of the state of foodborne illnesses in general in the developed world: They still happen but are today the exception rather than the rule. Recent lurid media coverage of foodborne illnesses might lead one to believe that it represents a growing epidemic. However, the Centers for Disease Control and Prevention’s (CDC) FoodNet program shows that most types of foodborne illnesses have declined since the late 1990s.2
If serious foodborne illnesses are rarer than ever in the developed world, mild cases are still all too common, and the potential for deadly consequences is always present: One in six Americans (48 million) will contract a foodborne illness this year3 — with 128,000 of those cases requiring hospitalization and roughly 3,000 of them ending up fatal. Outside the developed areas of the world, foodborne illnesses remain a major public health threat. Without widespread use of refrigeration or proper food-handling procedures, food spoilage is a much bigger issue. A recent report from the World Health Organization estimated 2.2 million deaths a year from diarrhea alone.4
Although over-the-top media coverage may be partially responsible for the public perception that food poisoning is on the rise, there is also the fact that modern transportation — in which fresh food can be quickly distributed farther from its point of origin than ever — can lead to foodborne illness outbreaks covering more territory than was possible in earlier generations. A recent outbreak of Listeria contained in caramel-covered apples from a California producer led to infections in 11 states.5 And, even more recently in March, five patients at Via Christi St. Francis hospital in Wichita, Kan., contracted Listeria after consuming milkshakes with a single-serving Blue Bell ice cream product called Scoops. Three of those patients died.6
What Are Foodborne Illnesses?
While most diseases are defined by either the causative agent or the part of the body affected, foodborne illness refers to the entryway by which the disease enters the body. The national nonprofit advocacy organization STOP Foodborne Illness defines a foodborne illness as “an infection or irritation of the gastrointestinal (GI) tract caused by food or beverages that contain harmful bacteria, parasites, viruses or chemicals.” At the same time, botulism attacks the nervous system,7 prions cause brain-wasting disease,8 and hepatitis A attacks the liver9 — and all are clearly foodborne diseases. Therefore, a better definition might simply be any infection or poisoning caused by food or beverages containing harmful bacteria, parasites, viruses, toxins or chemicals. This is why there aren’t very many specialists in food poisoning — and why diagnosing a serious case of food poisoning can be challenging.
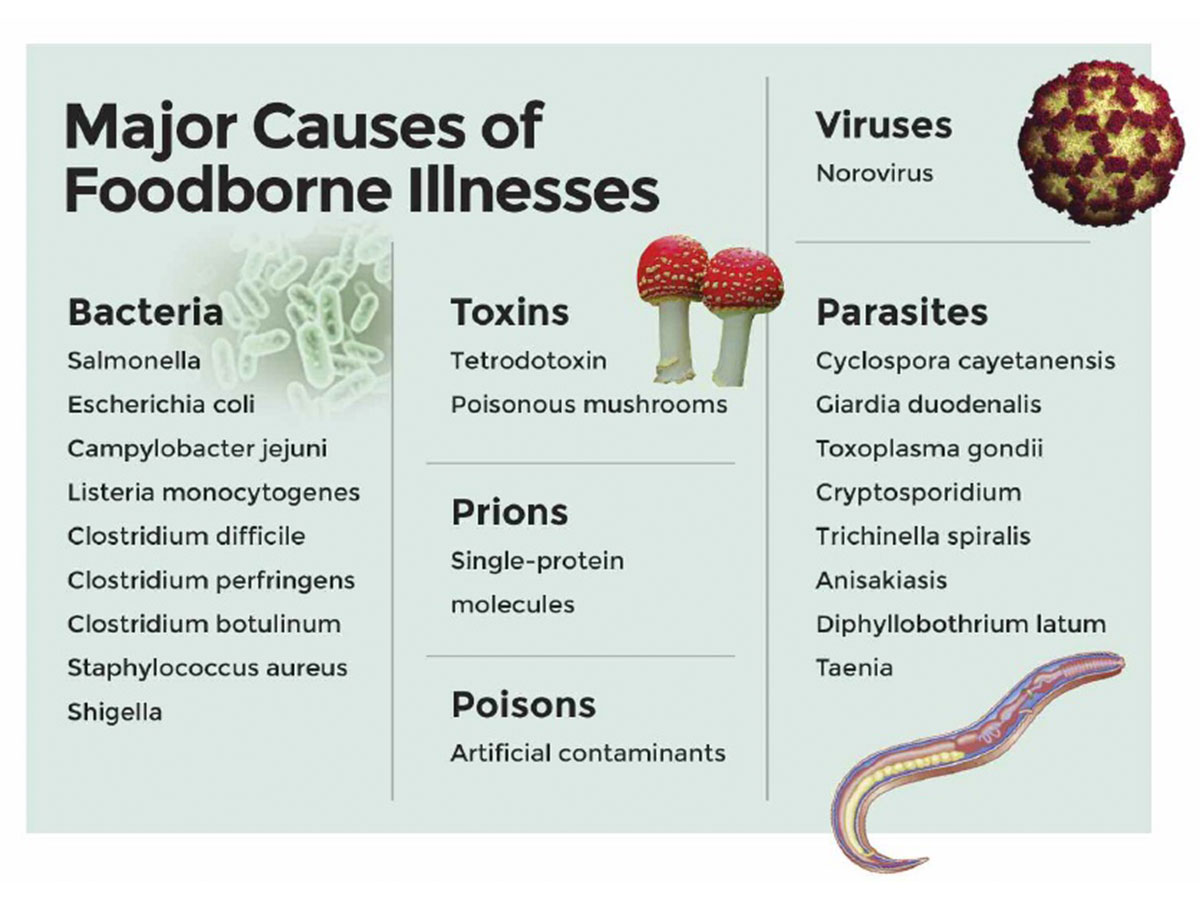
The major causes of foodborne illnesses are:
- bacteria
- viruses
- parasites
- toxins
- prions
- non-organic causes (poisons)
CDC reports that more than 250 types of foodborne illnesses have been identified,3 with causes ranging from defective proteins (prions) to bacterial toxins (Clostridium botulinum), mold to protozoa, and tapeworms to Trichinella spiralis.
Most cases of foodborne illness are entirely preventable. Bacteria, viruses and parasites in food sources can be killed by properly cooking food and eating it promptly. Refrigeration and freezing can slow or even prevent bacteria growth, while washing hands and keeping food covered can prevent outside bacteria from being introduced to food. Even pathogens like prions and toxins that cannot be killed or neutralized through cooking can be kept out of the food supply if standard foodhandling procedures (clean processing facilities, proper temperature control) are followed.
Symptoms, Diagnosis and Treatment
Most physicians will go their entire careers without ever seeing a patient suffering from botulism, Creutzfeldt-Jakob disease or tetrodotoxin poisoning. On the other hand, with one in six Americans contracting some sort of foodborne illness every year, all doctors will treat a case of food poisoning from time to time.
Fortunately, the least dangerous cases are also the most plentiful — and just a handful of CDC’s 250 sources of food poisoning are responsible for the vast majority of incidents in the U.S. Between them, norovirus, Salmonella, Campylobacter, Staphylococcus aureus and Clostridium account for some 91 percent of all food poisonings in the U.S. Toxoplasma gondii and Escherichia coli (E. coli) join norovirus, salmonella and Campylobacter in jointly causing 88 percent of foodborne illness-related hospitalizations, while Listeria replaces E. coli on the list of the top-five fatality-inducing foodborne illnesses in the U.S.3
The symptoms and diagnoses of these various agents can vary widely — as do, obviously, the treatments.
Viruses
CDC reports that almost 60 percent of all cases of food poisoning in the U.S. are caused by the norovirus.3 The virus attacks the stomach and intestines, causing inflammation that leads to cramping, nausea, diarrhea and vomiting. Infection usually lasts 72 hours or less. There are currently no antivirals available to treat norovirus, but most cases are not severe and are treated as with the flu: rest and plenty of liquids. CDC estimates that approximately 580 to 800 deaths a year in the U.S. are attributable to norovirus, mostly patients who are already weakened.10
Regular hand-washing before handling food and cooking food until it has an internal temperature above 140 degrees Fahrenheit are the best ways to prevent transmission of norovirus through food. The norovirus can be diagnosed by an RNA lab test of a stool sample.
Bacteria
Bacteria can cause disease either through infection, in which the bacteria themselves attack the host body’s cells, or through poisoning, in which the bacteria produce waste that is toxic to the host.
Salmonella causes more food poisonings in the U.S. than any other bacteria — being thought responsible for about 11 percent of all foodborne illness cases.3 As with the norovirus, the Salmonella bacteria attack the cells of the host’s stomach and/or intestines.11
There are two species of the Salmonella bacteria: Salmonella bongori, which is native to reptiles,12 and Salmonella enterica, which is naturally found in cattle and poultry (including chicken eggs).13 A subspecies of S. enterica is the cause of typhoid fever,14 which still kills about 160,000 people around the world every year15 (although almost none in the developed world; only about 5,700 cases are reported in the U.S. each year, with about three-quarters of them contracted duringoverseas travel16).
Symptoms of Salmonella are typical for those of any bacterial or viral food poisoning: abdominal cramps, diarrhea, vomiting, fever, headache and dehydration. Most cases are mild, and patients will self-treat without any medical intervention: rest, liquids and possibly a fever reducer. The infection usually runs its course in four to seven days.14
Serious cases — particularly those affecting infants, the elderly and those with weakened systems — may be treated with antibiotics. Diagnosis is made by inspecting a stool sample.17 Antibiotics used in treating salmonella include fluoroquinolones, third-generation cephalosporins and ampicillin. However, due to increased drug resistance seen in Salmonella bacteria, it is now recommended that antibiotics be used only in the most serious cases.18
Salmonella infections can be prevented by proper cooking of food, avoiding raw or undercooked foods, and washing hands thoroughly before handling food.
E. coli is a type of bacteria in the same family as Salmonella. These bacteria are one of the best-known types of foodborne illness-causing agents among the general public. Native to the digestive tracts of most warm-blooded organisms, E. coli are mostly harmless when left alone in the intestines. However, these bacteria can be transferred to the meat during meat processing. The strain E. coli O157:H7 is particularly virulent, causing cramps, bloody diarrhea and vomiting — and can also lead to kidney failure.19
E. coli can be ingested through raw produce or undercooked meat. A diagnosis is made through testing of a stool sample. There is not currently an antibiotic to treat an E. coli infection. Rest and fluids will help speed the body’s own recovery, and if the kidneys are attacked, dialysis may be employed to help.19
Campylobacter jejuni is the second most-common bacterial cause of foodborne illness in the U.S. Like S. enterica, Campylobacter jejuni is found naturally in poultry, and it causes about 10 percent of all cases each year. As with Salmonella, CDC believes most cases are never reported.20 Diagnosis is made by laboratory examination of a stool sample.
In Campylobacter jejuni infections, the bacteria attack the cells of the digestive system, causing diarrhea, fever, vomiting, nausea, dehydration, headache and muscle pain.20 However, some cases can lead to the development of Guillain-Barré syndrome. Researchers believe that the antibodies the immune system makes to fight Campylobacter jejuni bacteria attack the body’s own nerve cells after the infection has been defeated,21 which can lead to muscle weakness, paralysis and even death.22 This is extremely rare, however, and in most cases the Campylobacter infection runs its course in less than a week. In severe cases, or when the patient has high risk factors, the infection can be treated with azithromycin and fluoroquinolones. Again, drug resistance has been increasing in Campylobacter.
Listeriosis is the third most deadly of the bacterial foodborne infections,3 caused by the bacteria Listeria monocytogenes, a naturally occurring organism found in soil and water. This bacteria can be spread to humans through improperly handled or undercooked food. Listeria exists naturally in the environment all over the globe, and all humans are exposed to it. Generally, the elderly and others with compromised immune systems are the most likely to develop an infection. Symptoms include muscle ache, stiff neck, fever, diarrhea, confusion, loss of balance and/or confusion.23 Expecting mothers are also at heightened risk and can pass the disease to their babies. Diagnosis is generally made from a sample of spinal fluid. The recommended treatment is the antibiotic ampicillin, although trimethoprim/sulfamethoxazole, erythromycin, vancomycin, and the fluoroquinolones have also been used.24
Clostridium is a family of some 100 species of bacteria that causes a range of diseases from the rare but dangerous botulism to the healthcare-associated Clostridium difficile (C. difficile).
Clostridium perfringens causes about one-tenth of all cases of food poisoning in the U.S. It grows naturally, including in the digestive tracts of many animals, where it can be transferred to the meat during processing. The bacteria produce a toxin in the intestines of its host that causes the symptoms, which are generally cramping and diarrhea.25 Most infections last less than 24 hours, and CDC recommends against treating it with antibiotics. Diagnosis is made by a lab test on a stool sample.
The dangerous but rare botulism food poisoning is caused by toxins in food where Clostridium botulinumhas lived. The toxins affect the nervous system of humans who eat contaminated food, causing paralysis that can lead to death. Clostridium botulinum occurs naturally in the soil, including in areas where food crops are grown. Cooking food will kill the bacteria but not the toxins already created. CDC reports that fewer than 25 cases of foodborne botulism occur each year in the U.S., and most are the result of consuming home-canned foods that were improperly prepared (not using pressurized canning equipment to kill the bacteria before it can grow and excrete the toxin).26
The symptoms of botulism poisoning are drooping eyelids, double or blurry vision, slurred speech, difficulty swallowing and/or muscle weakness.27 Treatment will include use of an antitoxin kept on hand by CDC for distribution. Depending on the severity of the exposure, a patient may require a ventilator to assist with breathing until the paralysis begins to decrease, which can take weeks or even months. Total recovery takes years.26
Another bacteria that produces toxins that cause illness is Staphylococcus aureus, a common germ that lives on the skin and in the noses of otherwise healthy people. When the Staphylococcus aureus gets into food during preparation, however, it can create seven different compounds poisonous to humans.28 About 3 percent of cases of food poisoning in the U.S. are due to this agent.
Fortunately, the symptoms — appearing as soon as 30 minutes after eating contaminated food — are generally mild: nausea, vomiting, abdominal cramps and diarrhea. Few cases are formally diagnosed, according to CDC, because they can be treated with the usual rest and liquids. If a case is severe, or a wide foodborne outbreak is suspected and a diagnosis is warranted, a lab test of a stool sample can detect either the bacteria or the toxins. Antibiotics are not recommended.28
A rarer bacteria-caused foodborne or waterborne illness is Shigella. Most commonly seen in preschool-aged children, often in healthcare settings, it is generally passed when preparing food after contact with an infected person’s feces.28 The symptoms are generally confined to diarrhea that may contain blood. Most cases clear up within a week. More serious cases can be treated with trimethoprim-sulfamethoxazole, which is sold under the names of Bactrim, Septra or Cotrim. Due to increasing resistance to antibiotics seen in Shigella, the Mayo Clinic advises reserving antibiotic treatment for severe cases or for those patients with weakened immune systems.29
Parasites
Parasites are multicellular (tapeworms, roundworms) or large single-celled organisms (amoeba) that are ingested in food and then transfer to the host’s body to find their sustenance and safety. Most of these infections are the result of eating undercooked food or drinking untreated water.
The largest foodborne disease outbreak reported in the United States in 2013 was for Cyclospora in two possibly distinct outbreaks in Iowa-Nebraska and Texas.30 Cyclospora cayetanensis, which generally causes watery, explosive diarrhea, is caused by a single-celled organism that can only be diagnosed by examining a stool sample with a microscope.30 Treatment consists of the application of the antibiotics trimethoprim-sulfamethoxazole.32 The infection is usually traced to ingesting raw vegetables or to drinking untreated water. Recent outbreaks have been linked to produce imported to the U.S., although the U.S. Food and Drug Administration (FDA) reports that little is presently known about the microbe, including its natural habitat.33 It was virtually unknown before 1990.
Another single-celled organism that can cause infection in humans through contaminated meat or water is Giardia duodenalis. Symptoms are similar to those of bacterial GI infections: cramping, nausea, diarrhea and dehydration.33 As with most parasitic infections of the digestive tract, diagnosis is made by examining a stool sample in a lab. Treatment is generally with metronidazole, tinidazole or nitazoxanide, all of which will kill the parasite. None of these should be prescribed to pregnant women, however, due to the risks to the baby.
Toxoplasma gondii is a single-celled organism that can reproduce only while in the digestive tract of a cat.33 However, the infective reproductive cysts can be ingested by other animals, and humans can contract it through eating undercooked wild game, pork or lamb or by drinking untreated water. Most people who contract it will have no or very mild symptoms, including swollen lymph glands and muscle aches. However, unborn children exposed to it through their mother’s infections can develop serious, even fatal, complications. Those with compromised immune systems such as HIV patients can also develop very severe complications. (CDC has targeted toxoplasmosis as one of its five neglected parasitic infections.34) Once ingested, the parasite leaves the digestive tract and moves to muscle and nerve tissue. Diagnosis is performed by a blood test, looking for specific antibodies that indicate the presence of the parasite. Treatment consists of the antibiotics pyrimethamine and sulfadiazine, although most healthy patients will not need antibiotics.34
Cryptosporidium is a single-celled organism with a shell that can survive for long periods of time outside of a host. It is also resistant to chlorine (bleach). While generally transmitted via water, it can infect food during improper preparation.35 The symptoms are diarrhea and dehydration, and diagnosis is made by an exam of a stool sample. Most patients will recover with rest and fluids, while more severe cases can be treated with nitazoxanide.
Trichinosis is caused by the Trichinella spiralis, a roundworm ingested in undercooked wild game or, much left often today, domestic pork. The roundworms will complete their reproductive cycle in the intestines, then launch larvae into the bloodstream, where they will embed in muscle tissue, forming cysts.36 The first symptoms are similar to other types of foodborne illness: GI distress (cramping, vomiting and diarrhea). However, subsequent symptoms include eye swelling, headaches, aching joints and muscles, and general weakness. Because the worms migrate, a stool test may return a false negative; therefore, blood tests and muscle biopsies are more often used for a diagnosis.37 The antibiotics thiabendazole and mebendazole will kill the live adults in the digestive tract, but there is no treatment to kill the encysted larvae in muscle tissue.38
Anisakiasis is a roundworm found in fish and squid, and is contracted when eating infected fish or squid that have not been fully cooked.39 Symptoms are generic: abdominal cramping, nausea, diarrhea and vomiting. An endoscopic examination is used to diagnose an infection, and surgical removal of the worms is necessary in severe cases; mild cases will generally resolve on their own. However, the worm can migrate out of the digestive tract into the liver and even lungs, requiring surgical intervention in these cases.40
Diphyllobothrium latum is the largest parasite that can infect humans. A tapeworm, this species can grow up to 30 feet long.41 It is ingested in undercooked fish, and diagnosed through an examination of a stool sample. However, it is often asymptomatic for years, even decades, living in the host’s intestine and shedding millions of eggs a day.42 If symptoms do appear, they may include unexplained weight loss, abdominal pain or diarrhea. The worms can drop segments that migrate to the gallbladder or bile duct, causing infections to those organs.43 Praziquantel is most often prescribed for tapeworms. The drug causes the head of the tapeworm to detach from the intestinal wall, and the worm is then passed with the next bowel movement.
Taeniasis is a tapeworm infection caused by any one of three species of the genus Taenia. It is contracted by eating undercooked beef or pork infected with tapeworm, which then attaches to the host’s intestines.44 Symptoms are similar to those of the fish tapeworm: abdominal discomfort and weight loss. But as with other tapeworms, many people are unaware they are infected for years or decades. If oncospheres hatch in the intestines, they may migrate to muscle tissue or even the brain, causing cysticercosis, which can lead to seizures.45 As with other tapeworms, praziquantel is most often prescribed, along with niclosamide.
Toxins
While several of the bacteria listed above produce compounds that are poisonous to their human hosts after they are ingested, other toxins can be ingested that already exist within food. Perhaps the most infamous is tetrodotoxin, found in the puffer fish and related species popular in Japan and Japanese cuisine. Tetrodotoxin is confined to the liver and sex organs of the fish, and chefs in Japan must go through years of rigorous training and testing before they can prepare these species for human consumption.46 The toxin is heat-stable (so cooking will not neutralize it), and it is a deadly neurotoxin: There is no antidote, and as paralysis spreads through the body, the victim remains conscious the entire time.46 The symptoms — tingling and loss of muscle control — begin within minutes of ingestion, and the final outcome depends only on the size of the exposure.
Poisonous mushrooms continue to be a foodborne danger throughout the world, even in developed countries where hobbyists try to harvest wild species that may resemble edible or psychoactive varieties. As FDA warns, “there is no general rule of thumb for distinguishing edible mushrooms and poisonous toadstools.”47 Most toxins produced by mushrooms are heat-stable, meaning that cooking does not make them safer.
Because the symptoms vary by the species of poisonous mushroom, the government classifies mushroom poisonings into four physiological categories: protoplasmic (causing general decay of cells, resulting in organ failure), neurotoxins (affecting the nervous system), GI irritants (causing nonlethal discomfort such as nausea, diarrhea and cramping) and disulfiram-like toxins (which are only dangerous if consumed with alcohol).47
Of these four categories, the protoplasmic and neurotoxins are the most dangerous. One class of protoplasmic toxins, amanitins, is the only one that has a clinical test available commercially.47 The challenge for medical and emergency personnel is that, most often, a patient isn’t seen until a day or two has passed since ingestion, and the test has a two-hour turnaround. The amanitins can quickly lead to permanent, irreversible liver damage. Symptoms from these mushrooms often don’t appear for 12 hours after ingestion, at which time patients may experience persistent, violent vomiting, abdominal cramping and watery diarrhea. After a few hours, the symptoms will ease, leading patients to think they are well. Then, jaundice will manifest three to five days later, at which time a rapid decline in patient health may lead to coma and even death.
Prions
There is no general scientific consensus on just what prions are. They are smaller even than viruses, containing only a single protein molecule. What makes prions both dangerous and infectious is that they are misfolded proteins, and when near other similar proteins, they will cause them to misfold as well.48
Researchers have been aware of prion disease for several centuries, since ranchers first noticed a disease in sheep called scrapie. The affected sheep slowly became deranged, and it was clearly an infectious disease spreading from one sheep to another. Cows, too, can suffer from prion disease, most specifically bovine spongiform encephalopathy, popularly known as “mad cow disease.” The misfolded proteins tend to most resemble proteins on the surface of a nerve or brain cell, meaning that animals (including humans) with prion infection tend to suffer debilitating and ultimately fatal brain-wasting disease.
Prions are heat-stable, so cooking does not destroy them. The prions in an animal’s nervous system can be spread to the meat during the slaughtering and processing of the animals, which is how some humans developed variant Creutzfeldt-Jakob disease (vCJD) from eating infected meat.49 Symptoms of vCJD are similar to those of CJD, which is not believed to be associated with ingesting prions from infected food sources but is likely caused by spontaneous deformation of the proteins for unknown reasons.49 Patients will suffer significant personality changes, anxiety, depression, impaired thinking and blurred vision. Life expectancy is a little over a year from the onset of symptoms. There is no cure or treatment available.50 However, careful monitoring of livestock populations and improved care and feed protocols (no more mixing unused beef into cattle feed, or mutton into sheep feed) have mostly eliminated prion disease from our food sources.
Poisons
With much of our food supply being processed or packaged by automated factory equipment, occasionally artificial contaminants are introduced into our food, and many of these can act as toxins to the human body. If produce isn’t properly rinsed, pesticide residue may remain. Trace amounts of artificial hormones may also remain in meat and poultry and have deleterious effects on those who consume them. Harvesting machines may accidentally introduce lubricants onto crops headed for the table, or canning equipment may have cleaning residue.51
FDA maintains information on different chemicals that can accidentally enter the food supply. Local poison control centers and emergency rooms have information on nearly all of these compounds, their symptoms and appropriate treatments.
Prevention and Research
Not only are nearly all cases of foodborne illnesses preventable, but most foodborne illness outbreaks are now required to be reported to public health authorities.52 If a physician suspects the possibility of food poisoning, they are able to check with local public health authorities or the CDC’s FoodNet to see if a foodborne illness has been reported in that area. If so, the physician can then follow up with the patient to see if he or she may have been exposed to the reported outbreak, which can provide guidance in determining the diagnosis and treatment.
Refrigeration, proper cooking and cleanliness remain the best ways to prevent foodborne illness. The food supply in the U.S. is regulated both by law and by industry guidelines. From livestock ranches to lettuce farms, from distribution centers to refrigerated railcars and semitrailers, from grocery stores to farmers markets to restaurants, there are both written regulations and well-understood best practices that help protect our food chain from disease-causing agents.
When a patient does contract a foodborne illness, particularly from a meal prepared at home, it may be advisable to review basics of food safety with them:
- Always fully cook meat, poultry and eggs (a meat thermometer is the only way to be sure a meal is fully cooked); learn the temperature each kind of meat should be cooked to ensure safety.53
- Always wash hands with hot water and soap before handling any food, or when handling dishes or utensils that will touch food.
- Keep produce and meats refrigerated when not in use. Don’t leave food to thaw on the countertop or leave prepared food out longer than a few hours (it’s not just meat — even fresh produce that has been sliced can host dangerous pathogens if left at room temperature for more than a few hours).
- Be sure the refrigerator is working properly and that it is chilled to 40 degrees Fahrenheit or cooler.54
It’s important to remind patients that food left out too long at room temperature may be infected by bacteria that produce poisons that won’t be removed by cooking and that remain dangerous even if the bacteria are killed by heating (cooking) the food.54 CDC has designated foodborne illnesses as one of its “winnable battles,” and is putting considerable resources into further strengthening the protective measures surrounding our food supply.55 Among the strategies being used to combat foodborne illnesses are:
- Improved communication with state and local health agencies
- New technology in public health labs to help identify sources of food-based infection more quickly
- Better food surveillance systems and improved data sharing when an outbreak is reported or detected56
Given that food fit for humans is also food fit for bacteria, viruses, mold, parasites and just about anything living, it is unlikely that we can ever wholly eradicate foodborne illness. But by working with ranchers, farmers, distributors, grocers, restaurateurs and the general public in emphasizing the importance of following proven best practices in food handling, and combining that with improved detection and communication, it does seem likely that we can continue to reduce incidences of foodborne illness and ensure they remain the rare exception to our safe food supply.
References
- American Cancer Society. Stomach Cancer Overview. Accessed at www.cancer.org/acs/groups/cid/documents/webcontent/003077-pdf.
- Centers for Disease Control and Prevention. Food-borne Diseases Active Surveillance Network (FoodNet) Tables and Figures – 2013 Preliminary Data. Accessed at www.cdc.gov/foodnet/data/trends/tables-2013.html.
- Centers for Disease Control and Prevention. Foodborne Illness, Foodborne Disease. Accessed at www.cdc.gov/foodsafety/facts.html.
- Dewaal CS, Robert M, Witmer J, and Tian XA. A Comparison of the Burden of Foodborne and Waterborne Diseases in Three World Regions, 2008. Accessed at cspinet.org/new/pdf/food_protection_trends__aug._2010.pdf.
- U.S. Food & Drug Administration. Bidart Bros. Works with Federal and State Officials to Determine Source of Listeriosis-Associated Outbreak. Recall – Firm Press Release, Jan. 9, 2015. Accessed at www.fda.gov/Safety/Recalls/ucm429689.htm.
- 3 Kansas Hospital Patients Die from Ice Cream Contamination. FoxNews.com, March 14, 2015. Accessed at www.foxnews.com/health/2015/03/14/3-kansas-hospital-patients-die-from-ice-cream-contamination.
- Centers for Disease Control and Prevention. Facts About Botulism. Accessed at www.bt.cdc.gov/agent/botulism/factsheet.asp.
- Centers for Disease Control and Prevention. Prion Diseases. Accessed at www.cdc.gov/ncidod/dvrd/prions.
- Mayo Clinic. Hepatitis A. Accessed at www.mayoclinic.org/diseases-conditions/hepatitis-a/basics/causes/con-20022163.
- Centers for Disease Control and Prevention. Norovirus. Accessed at www.cdc.gov/norovirus/about/overview.html.
- Netdoctor. Salmonella and food poisoning. Accessed at www.netdoctor.co.uk/health_advice/facts/salmonella.htm.
- Wikipedia. Salmonella bongori. Accessed at en.wikipedia.org/wiki/Salmonella_bongori.
- Wikipedia. Salmonella enterica. Accessed at en.wikipedia.org/wiki/Salmonella_enterica.
- Medline Plus. Salmonella Infections. Accessed at www.nlm.nih.gov/medlineplus/salmonellainfections.html.
- Wikipedia. Typhoid Fever. Accessed at en.wikipedia.org/wiki/Typhoid_fever.
- Centers for Disease Control and Prevention. Typhoid Fever. Accessed at www.cdc.gov/nczved/divisions/dfbmd/diseases/typhoid_fever.
- Centers for Disease Control and Prevention. Salmonella: Diagnosis and Treatment. Accessed at www.cdc.gov/salmonella/general/diagnosis.html.
- Medscape. Salmonellosis Treatment & Management. Accessed at emedicine.medscape.com/article/228174-treatment.
- Mayo Clinic. E. Coli Definition. Accessed at www.mayoclinic.org/diseases-conditions/e-coli/basics/definition/con-20032105.
- Foodborne Illness. Campylobacter. Accessed at www.foodborneillness.com/campylobacter_food_poisoning.
- Nachamkin I, Allos BM, and Ho T. Campylobacter Species and Guillain-Barré Syndrome. Clinical Microbiology Reviews, 1998;11(3):555-567. Accessed at www.ncbi.nlm.nih.gov/pmc/articles/PMC88896.
- National Institute of Neurological Disorders and Stroke. Guillain-Barré Syndrome Fact Sheet. Accessed at www.ninds.nih.gov/disorders/gbs/detail_gbs.htm.
- Centers for Disease Control and Prevention. Listeria (Listeriosis) Definition. Accessed at www.cdc.gov/listeria/definition.html.
- Temple ME, and Nahata MC. Treatment of Listeria. Annals of Pharmacotherapy. 2000 May;34(5):656-61. Accessed at www.ncbi.nlm.nih.gov/pubmed/10852095.
- Centers for Disease Control and Prevention. Clostridium perfringens. Accessed at www.cdc.gov/foodsafety/clostridium-perfingens.html.
- Centers for Disease Control & Prevention National Center for Emerging and Zoonotic Infectious Diseases. Botulism. Accessed at www.cdc.gov/nczved/divisions/dfbmd/diseases/botulism.
- Centers for Disease Control and Prevention. Home Canning and Botulism. Accessed at www.cdc.gov/features/HomeCanning.
- Centers for Disease Control and Prevention. Staphylococcal Food Poisoning. Accessed at www.cdc.gov/ncidod/dbmd/diseaseinfo/staphylococcus_food_g.htm.
- Mayo Clinic. Shigella Infection. Accessed at www.mayoclinic.org/diseases-conditions/shigella/basics/definition/con-20028418.
- Andrews J. The 10 Biggest Food-borne Illness Outbreaks of 2013, Food Safety News, Dec. 27, 2013. Accessed at www.foodsafetynews.com/2013/12/the-10-biggest-u-s-outbreaksof-2013/#.VM7FG2jF-So.
- Mayo Clinic. Cyclospora infection. Accessed at www.mayoclinic.org/diseases-conditions/cyclospora/basics/definition/con-20032789.
- Centers for Disease Control and Prevention. Parasites: Food. Accessed at www.cdc.gov/parasites/food.html.
- United States Department of Agriculture. Parasites and Foodborne Illness. Accessed at www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/get-answers/food-safety-fact-sheets/foodborne-illness-and-disease/parasites-and-foodborne-illness.
- Centers for Disease Control and Prevention. Parasites – Toxoplasmosis (Toxoplasma infection). Accessed at www.cdc.gov/parasites/toxoplasmosis/index.html.
- Centers for Disease Control and Prevention. Parasites – Cryptosporidium (also known as ‘Crypto’). Accessed at www.cdc.gov/parasites/crypto/index.html.
- Centers for Disease Control and Prevention. Parasites – Trichinellosis (also known as Trichinosis). Accessed at www.cdc.gov/parasites/trichinellosis/biology.html.
- Mayo Clinic. Trichinosis: Tests and Diagnosis. Accessed at www.mayoclinic.org/diseasesconditions/trichinosis/basics/tests-diagnosis/con-20027095.
- Michigan State University. Treatment and Prevention of Trichinella Spiralis. Accessed at www.msu.edu/course/zol/316/tspitreat.htm.
- Centers for Disease Control and Prevention. Parasites – Anisakiasis. Accessed at www.cdc.gov/parasites/anisakiasis/index.html.
- Sakanari JA, and McKerrow, JH. Anisakiasis. Clinical Microbiology Reviews, 1989 Jul; 2(3):278–284. Accessed at www.ncbi.nlm.nih.gov/pmc/articles/PMC358121.
- Centers for Disease Control and Prevention. Parasites – Diphyllobothrium Infection. Accessed at www.cdc.gov/parasites/diphyllobothrium/index.html.
- Parasites in Humans. Diphyllobothrium Latum – Fish Tapeworm. Accessed at www.parasitesinhumans.org/diphyllobothrium-latum-fish-tapeworm.html.
- Centers for Disease Control and Prevention. Diphyllobothriasis. Accessed at www.cdc.gov/dpdx/diphyllobothriasis.
- Centers for Disease Control and Prevention. Parasites – Taeniasis. Accessed at www.cdc.gov/parasites/taeniasis/index.html.
- Centers for Disease Control and Prevention. Parasites – Cysticercosis. Accessed at www.cdc.gov/parasites/cysticercosis/biology.html.
- Buerk R. Fugu: The Fish More Poisonous Than Cyanide. BBC News Magazine, May 17, 2012. Accessed at www.bbc.com/news/magazine-18065372.
- U.S. Food and Drug Administration. BBB Mushroom Toxins. Accessed at www.fda.gov/Food/FoodborneIllnessContaminants/CausesOfIllnessBadBugBook/ucm070853.htm.
- Prion Alliance. What Are Prions? Nov. 26, 2013. Accessed at www.prionalliance.org/?s=What+are+prions&submit=Search.
- Centers for Disease Control and Prevention. About vCJD. Accessed at www.cdc.gov/ncidod/dvrd/vcjd/index.htm.
- Mayo Clinic. Creutzfeldt-Jakob disease. Accessed at www.mayoclinic.org/diseases-conditions/creutzfeldt-jakob-disease/basics/symptoms/con-20028005.
- U.S. Food and Drug Administration. Chemical Contaminants, Metals, Natural Toxins & Pesticides Guidance Documents & Regulations. Accessed at www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/ChemicalContaminantsMetalsNaturalToxinsPesticides/default.htm.
- Centers for Disease Control and Prevention. About FoodNet. Accessed at www.cdc.gov/foodnet/about.html.
- STOP Food-borne Illness. Safe Cooking Temperatures. Accessed at www.stopfoodborneillness.org/safe-cooking-temperatures.
- U.S. Food and Drug Administration. Refrigerator Thermometers: Cold Facts About Food Safety. Accessed at www.fda.gov/Food/ResourcesForYou/Consumers/ucm253954.htm.
- Centers for Disease Control and Prevention. Food Safety. Accessed at www.cdc.gov/WinnableBattles/FoodSafety/index.html.
- Centers for Disease Control and Prevention. Food Safety: A CDC Winnable Battle. Accessed at www.cdc.gov/winnablebattles/foodsafety/pdf/foodsafety_wb_at_a_glance.pdf.