Data Collection: A New Regime
- By Bonnie Kirschenbaum, MS, FASHP, FCSHP
An ongoing revolution in healthcare inexplicitly ties data and reimbursement with the demand for analytics that provide insight into a variety of areas — from treatment to business intelligence vital to the management of healthcare organizations and practices. The significant changes the healthcare industry experienced in 2015, ranging from reimbursement reform philosophy to coding changes inherent to the adoption of ICD-10, continue. Vital to keeping pace includes closing the gaps between areas of technology with no sector left behind. For instance, in some practices, the clinical component surges ahead, while the billing department churns out snailmail paper bills. In hospital settings, some critical care and inpatient areas are reaping IT dollars with the latest and greatest systems, while outpatient areas are left with antiquated electronics and IT tools with limited or no interoperability.
Analytics turn data into usable information, which is not surprising as more and more data are collected in response to the mandated growth of electronic health records. What is surprising is an announcement by Andy Slavitt, acting administrator for the Centers for Medicare and Medicaid Services (CMS), on Jan. 12 confirming the Meaningful Use program will end sometime in 2016, and it will be replaced by something better. “Now that we effectively have technology in virtually every place where care is provided, we’re now in the process of ending Meaningful Use and moving to a new regime culminating with the MACRA implementation,” advised Slavitt. MACRA, the Medicare Access and CHIP Reauthorization Act of 2015, authorized new payment models for providers, including the Merit-Based Incentive Payment System (MIPS).
The details of this new regime are yet to be released, but the goal is to move away from rewarding providers for using technology toward achieving good patient outcomes by letting providers customize their goals so that technology is built around individual practice needs. The underlying message is that technology is essential to achieving those good patient outcomes. Slavitt emphasized the value of start-up companies, including use of open APIs (application programming interfaces) “to open the physician desktop and allow apps, analytic tools and connected technologies to get data in and out of information systems securely.” CMS is “deadly serious about interoperability.” “Better interoperability is necessary to close referral loops and engage patients in their care,” Slavitt noted, “and data blockers will not be tolerated.”
It’s clear there is a need for trained professionals who know how to work with data to become an integral part of healthcare organizations to leverage the use of data and make data-based decisions. New healthcare payment reform models are based on collaboration, and the sharing of useful clinical or business data that are produced by analytics is an essential tool.
As healthcare practices launch into the 2016 payment year, the questions they should ask are: 1) Are we doing the things needed to better manage what’s coming? 2) What is the impact to cost, quality and outcomes metrics of using an inadequate charge description master (CDM) with poor descriptions? 3) Does our team think of themselves as a value cycle team and make decisions that support that concept? 4) Have we elevated the priority of fixing problems, and do the CFO and finance team know what these problems are? 5) Where are the gaps, and how are we going to manage them? 6) What opportunities do they present?
At the Dec. 1 CMS Quality Conference in Baltimore, Slavitt stressed that CMS will adopt a value-based payment policy as part of an attempt at industrywide delivery system reform: “Our priority is clear: to drive a delivery system that provides better care with a smarter payment system that keeps people healthier. This means specifically that by 2018, we will reach a tipping point in our payments with over 50 percent of Medicare fee-for-service payments rewarding for quality and value and aligning Medicare Advantage and Medicaid to do the same.” Slavitt also emphasized that payment policy alone is not CMS’ goal: “We are not just a payer; we are an information partner.… The agency wants to turn healthcare into an information industry that supports patients and the caregivers that serve them.”
As such, providers and organizations must concentrate on the importance of telling patients’ stories accurately and completely in a manner that can be coded appropriately for reimbursement purposes and for contributing to the “big data pool.” Their responsibility is to understand the nuances of the payment reform rules and proposals and put them into play at their facility to be a data champion. This means embracing the concept that CMS is not just a payer but a data repository and information partner. CMS, like all payers, collects a wealth of information about patients through the data that facilities send through its claims submissions.
It’s important to note that there is a difference between local data warehouses at a facility level that retain data to support analytics and bigger centralized datasets that constitute the big data pool used by regulators, payers and large delivery systems. At a facility level, it’s possible that everything recorded is retrievable from the data warehouse. However, only claims data currently populates CMS and most other payer databases. With this in mind, developing strategies for managing data requires a variety of tactics to ensure patients’ stories are told completely and accurately.
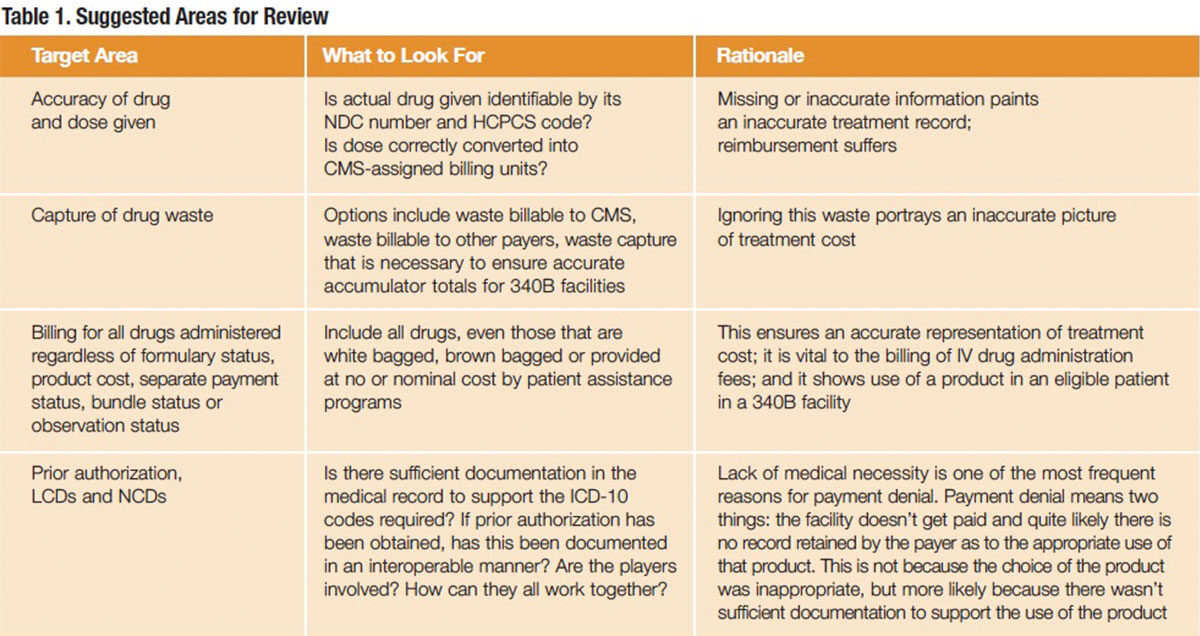
Since the majority of healthcare payment reform centers on a shift from the inpatient to the outpatient setting and coordination among a variety of caregivers, the suggested areas for review in Table 1 are directed at that environment and refer to the Outpatient Prospective Payment System rules for 2016. These suggestions for review can be used to ensure that data management is working to support these goals. It’s often a surprise what gets removed from submissions as they wend their way through the tortuous twists and turns of revenue cycle software systems. A little education will go a long way to resolving many of these issues.
Editor’s Note: The content of this column is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.