Renal Failure
Chronic and acute kidney failure can be the result of many causes, and its prevalence is growing at historic rates, but it is no longer a death sentence.
- By Jim Trageser
Engineers like to speak of “mission critical” components in various systems — components so key to the overall operation that their failure can cause the entire system to become unstable or halt. The human body has quite a few mission critical components: the brain, the heart, the liver and the kidneys. If any of these stop working, life ceases. Nature utilizes a concept engineers refer to as “redundancy” — components that are repeated in the system for safety so that if one fails, the rest can continue to function and keep the system operating. The lungs are a prime example of redundancy in the human body. Kidneys are another, with their role in clearing the bloodstream of toxins. If one is damaged, the other can continue functioning. Unfortunately, most of the nontraumatic causes of renal failure are likely to affect both kidneys.
What Is Renal Failure?
The medical community classifies kidney failure into two general categories: chronic kidney disease (CKD) and acute kidney disease. Both describe a condition in which the ability of one or both kidneys to effectively filter the blood has been weakened, leading to a buildup of toxins in the body.1
Chronic kidney failure is a slow-developing condition that can exist for years before it is detected. It is generally caused by other health issues such as diabetes or hypertension.2
Acute kidney failure can develop over the course of days or even hours. It is most often the result of traumatic injury to the kidneys (from an auto accident, for instance) or other sudden health emergency: a heart attack, liver failure, infection.3 End-stage renal disease (ESRD) occurs when the kidneys are irreversibly damaged, requiring dialysis and/or transplant. This can result from either chronic or acute kidney failure when the kidneys have 10 percent or less of healthy function.4
The Centers for Disease Control and Prevention reports that kidney failure is the No. 9 cause of death in the United States, with some 47,000 patients dying from kidney failure in 2013.5 A total of 3.9 million people were diagnosed with kidney disease that year in the United States (about 1.7 percent of the total population). Other studies indicate that up to 20 million adults (one in 10) have undiagnosed kidney disease.6
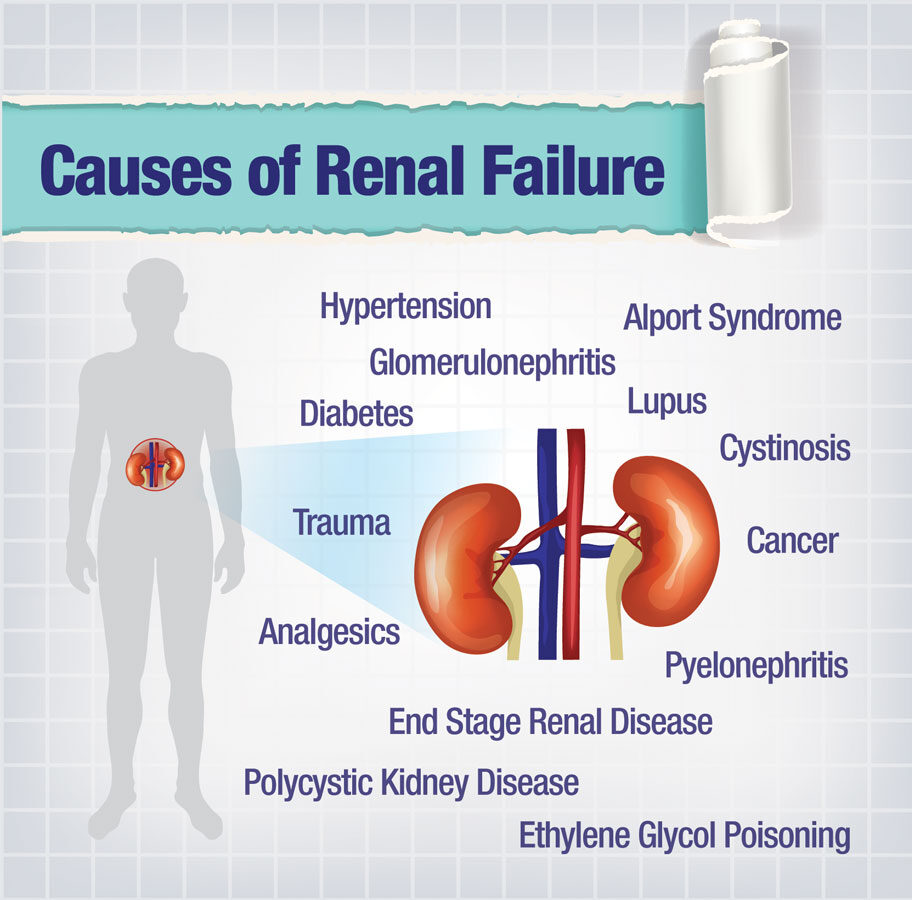
Causes of Renal Failure
Kidney disease and failure can be brought on by many different conditions, from cancer to infection. However, the vast majority of cases are attributed to diabetes and hypertension. In the United States, diabetes alone accounts for 44 percent of all cases of kidney failure, while hypertension causes about 28 percent.6
Other top causes in the U.S. include glomerulonephritis (an inflammation of the glomeruli, the tiny filters that remove waste from the bloodstream), kidney infections, lupus and other autoimmune diseases, kidney stones, polycystic kidney disease (a hereditary disease in which cysts develop on the kidneys, impairing their function), overuse of some pain medications, and abusing illegal drugs.6 Physical trauma — a kidney being punctured or severely bruised by an accident, sports, etc. — can also trigger kidney disease or failure.
Symptoms of Renal Failure
The onset of kidney disease can manifest through a variety of symptoms, no matter the underlying cause:7
- Changes in urine output
- Nausea and/or vomiting
- Swelling due to fluid retention
- Fatigue
- Chest pain
- Confusion
- Changes in sleeping patterns
Of course, these symptoms may also indicate other conditions as well. And in many cases, kidney disease will have no symptoms and is only detected through lab tests — sometimes lab tests looking for other conditions.7,8 Unfortunately, at this point, there may already be serious, permanent damage to kidney function before the disease is diagnosed.
Diagnosing Renal Failure
Several tools can be used to make a formal diagnosis of kidney disease:
- Urine tests: Lab tests of a urine sample can look for excessive levels of proteins, blood and/or sugar. High protein levels can indicate that the kidneys are not functioning properly, while high blood sugar levels can help detect underlying causes of low kidney function such as diabetes.9
- Blood tests: The results of blood sample tests can show elevated levels of creatinine and urea nitrogen, toxins that are removed from the bloodstream by healthy kidneys.9
- Imaging: Both ultrasounds and CT scans can reveal physical abnormalities in the kidneys, or kidney stones.9
- Biopsy: Kidney tissue can be tested for infecting organisms, high protein levels or other symptoms or causes of kidney disease. It may also be prescribed in cases where a transplanted kidney is not doing well.10
Treating Renal Failure
Once a positive diagnosis of kidney disease has been made, treatment options depend on the amount of damage to the kidneys, whether that damage is permanent and the underlying cause of the disease. While treating the root cause of the kidney dysfunction is the only way to halt or at least slow the advance of the damage to the kidneys, physicians also need to address patient symptoms to relieve pain and stress.
Symptomatic relief may include:
- Diuretics to reduce swelling due to fluid retention11
- Iron or hormone treatments to treat anemia; erythropoietin is a common hormone supplement used to treat anemia associated with CKD10
- Calcium or vitamin D supplements to prevent bone damage11
- Drugs to control the potassium levels in the blood; sodium polystyrene sulfonate (often sold as Kayexalate or Kionex) is commonly prescribed if potassium levels are high (which can cause irregular heartbeat or muscle weakness)12
Diabetes causes kidney damage when high sugar levels cause the kidneys to filter more blood than normal, increasing the wear and tear on the glomeruli, which are specialized capillaries. As these tiny filters wear out, the kidneys become less effective, leaving more waste in the bloodstream.
Despite the sobering statistics, kidney disease is not inevitable with diabetes. Diabetics can prevent or slow the advance of kidney disease by carefully regulating their blood sugar levels and controlling their blood pressure. Weight control, avoiding alcohol and tobacco, and regular exercise are all key components of controlling diabetes-related hypertension (or any hypertension). Some physicians prescribe a low-protein diet, as that seems to slow the progression of kidney disease by lessening the amount of work for the kidneys.13
A class of drugs known as ACE inhibitors (angiotensin-converting enzyme inhibitors) is also often used in conjunction with one or more of the above approaches. These drugs not only lower blood pressure by blocking release of an enzyme that constricts blood vessels, but also seem to preserve kidney function in ways other blood pressure medications do not.14 The literature indicates that researchers are not entirely clear as to why this works, but studies show that there is a clear benefit to using ACE inhibitors for diabetics with CKD.
Hypertension can lead to kidney disease by slowly stretching out the glomeruli. As the glomeruli enlarge, their ability to filter out toxins while leaving healthy cells and nutrients in the bloodstream becomes compromised. For those with hypertension linked to diabetes, these effects compound the damage done by blood sugar levels associated with diabetes. But even in cases where high blood pressure is not related to diabetes, the treatment is the same: improved diet and exercise and, if necessary, a regimen of hypertension medication — generally ACE inhibitors.
Lupus can cause kidney disease when the body’s immune system attacks the kidneys, causing inflammation of the glomeruli and a related structure called the nephron — a condition known as glomerulonephritis that prevents the kidneys from effectively filtering the blood. Glomerulonephritis is very common in lupus patients, with up to 40 percent of adults and 67 percent of children developing kidney disease. Kidney disease associated with lupus may be treated with prednisone or other corticosteroids to reduce swelling and restore kidney function.15 These medications may be supplemented by or even replaced by immunosuppressive drugs such as cyclophosphamide (Cytoxan), azathioprine (Imuran), cyclosporin A and mycophenolate mofetil (CellCept). To complicate matters, other medications used to treat lupus can create side effects that mimic the symptoms of CKD. And, long-term use of nonsteroidal anti-inflammatory drugs or aspirin to treat the symptoms of lupus can lead to CKD.
Glomerulonephritis has many causes besides lupus: Strep throat can lead to the development of glomerulonephritis, as can Goodpasture’s syndrome, Wegener’s granulomatosis and polyarteritis nodosa. When glomerulonephritis develops from one of these causes, it is generally considered an acute kidney disease. In each of these diseases, the underlying cause must be addressed in order to treat the kidney disease.
Post-streptococcal glomerulonephritis is caused by an untreated strep infection. It generally manifests about two weeks after a throat infection, and three to four weeks after a skin infection. It will usually subside on its own in a few weeks to a month. Antibiotics should be used to kill off any remaining streptococcal bacteria, and diuretics can help relieve any swelling from fluid retention. However, corticosteroids and other anti-inflammatory medications generally are ineffective.16
Goodpasture’s syndrome is an autoimmune disease of unknown cause, in which the immune system produces antiglomerular basement membrane (GBM) antibodies that attack a collagen that helps make up the glomeruli. It can be successfully treated with corticosteroids, immunosuppressives such as cyclophosphamide to lower the number of antibodies being created and, in severe cases, plasmapheresis, which removes the GBM antibodies from the patient’s blood supply.17
Wegener’s granulomatosis is a rare inflammation of the blood vessels that results in restricted blood flow that damages the kidneys. While the cause is presently unknown, research indicates it is likely an autoimmune disorder.18 It is treated with prednisone and other corticosteroids, along with immunosuppressives — cyclophosphamide (Cytoxan), azathioprine (Azasan, Imuran) or methotrexate (Rheumatrex, Trexall) — which help stop the body’s attack on itself.19
Polyarteritis nodosa is an inflammation of the arteries, the cause of which is presently unknown. However, it can be effectively treated with high doses of corticosteroids in most cases. More severe cases can be treated with immunosuppressives.20
Glomerulonephritis can also be chronic, developing slowly. It is known to run in families and to not have a definable cause in some patients. This chronic form often takes years to show symptoms. There is no specific treatment for chronic glomerulonephritis; however, dietary restrictions (limiting intake of salt, protein and potassium) can help, as can controlling hypertension.21
Polycystic kidney disease (PKD) is a hereditary condition in which benign cysts grow in and on the kidneys. There is no cure. Keeping hypertension under control is critical — usually with ACE inhibitors. Pain from the cysts may be treated with acetaminophen. If the pain becomes unbearable, or if the cysts obstruct blood vessels or other organs, surgery may become necessary. Most patients with PKD will eventually progress to ESRD and need dialysis or transplant.22
Cystinosis is a genetic disease that causes an intracellular buildup of the amino acid cystine.23 The condition is successfully treated with Cysteamine, which removes the cystine from cells.24
Alport syndrome is a genetic disease that leads to kidney disease due to the lack of a needed protein to make collagen.25 Without collagen, the glomeruli that serve as filters are not replaced or repaired as needed, and they lose their ability to effectively filter the blood. There is no cure, but the progression of the disease can be slowed by carefully controlling blood pressure.
Cancer can originate in the kidneys (kidney cancer) or spread to the kidneys from another malignancy. The American Cancer Society reports that renal cancer is one of the 10 most common forms of cancer for both men and women.26 In adults, the most common form is renal cell carcinoma. Young children are more prone to a type of malignancy called Wilms’ tumor. Treatment will depend on how advanced the cancer is, the specific form of cancer, where on the kidney it is located and the age of the patient. Strategies include surgery, radiation and chemotherapy — often a combination of these. Depending on how renal performance is affected, dialysis may also be part of the treatment.
Pyelonephritis is an infection of the urinary tract that, if left untreated, can cause scarring in the kidneys, potentially leading to kidney failure. While many bacteria and viruses can cause pyelonephritis, the most common culprit is E. coli.27 Treatment generally consists of a round of antibiotics with bed rest and plenty of fluids.
Some analgesics can cause chronic interstitial nephritis (a swelling of the tubules that return water and nutrients to the bloodstream after filtering) if used long term. Ibuprofen and naproxen are among them. And high doses of aspirin taken for a long time can also lead to this condition. (Low doses of daily aspirin used to prevent heart attacks are safe.)28
Ethylene glycol poisoning can bring about kidney failure in a matter of hours. Patients suspected of ingesting ethylene glycol, a common ingredient in automotive antifreeze, should immediately be sent to the nearest emergency room, where their stomach can be pumped and, in many cases, they will be hooked up to a dialysis machine to remove the poison from the bloodstream.29 Illegal street drugs, including heroin, phencyclidine (PCP) and MDMA (3,4- methylenedioxymethamphetamine), can also damage or destroy kidney function.30As there is no other treatment to restore kidney function in cases of poisoning, the kidneys will either heal with time, or the damage is irreversible.
Trauma to the kidneys can occur in a variety of settings, from sports injuries to car accidents to battlefield wounds. Advances in treatment mean there are options beyond surgical removal of a damaged kidney. For example, embolization and endourologic stenting to control bleeding are both nonsurgical methods of treatment. As always, though, the specific nature and severity of the injuries will determine the correct treatment path.
ESRD occurs when kidneys have less than 10 percent of normal function left. At this point, the body needs assistance ridding itself of toxins. There are two treatments for ESRD: transplant and dialysis. Due to demand, wait times for a donor kidney can stretch into years. And due to underlying health or lifestyle issues, some patients are not candidates for transplant. In transplant, the healthy kidney of a donor — living or deceased — is matched for compatibility. In general, the existing kidneys are kept in place, and the new kidney is placed adjacent to them. Antirejection drugs are prescribed to prevent the patient’s immune system from attacking the foreign organ.
There are two types of dialysis. Hemodialysis uses a tube to run the blood supply through the dialysis machine, artificially performing the work of the kidneys to remove toxins. Peritoneal dialysis uses a tube to pump a solution into the abdominal cavity to absorb waste products, which can then be withdrawn and disposed of.11
Preventing Renal Failure
Many cases of kidney disease are preventable. While nearly three-quarters of kidney disease in the United States is linked to diabetes or hypertension, neither condition makes kidney disease an inevitability.
Kidney damage that leads to kidney disease and failure can be prevented through good health maintenance: avoiding smoking and alcohol (or drinking in moderation), avoiding illegal street drugs, keeping blood pressure under control and avoiding over-reliance on analgesics. Even if these steps do not prevent kidney damage due to diabetes or other underlying health issues (lupus, hypertension), they will help relieve the stress on the kidneys and slow the progression of kidney disease.
Ongoing Research
Currently, much research is concentrated on multiple fronts to develop better technologies and treatments for kidney disease.
Benjamin Freedman, a researcher at Brigham and Women’s Hospital and Harvard Medical School, is working with adult stem cells of patients with polycystic kidney disease to study the cellular-level nature of PKD to see if treatments can be developed — or perhaps even a cure.31 The hope is that Freedman’s research will lead to a method of taking kidney cells from PKD patients, then genetically engineering those cells to be free of the genetic mutation that causes PKD before reintroducing them into the patient’s kidneys.
Dr. Marta Christov from Massachusetts General Hospital is working on new methods of removing phosphorus from the body to help slow skeletal and vascular damage in those suffering from CKD.32
Another researcher at Mass General, Dr. Sahir Kalim, is conducting research to improve the efficiency of dialysis so that it more closely mirrors the work done by healthy kidneys. Even the best dialysis machines today remove too many amino acids and miss too many metabolites.33
And Dr. Martina McGrath, at Brigham and Women’s Hospital in Boston, is exploring new strategies to further reduce rejection of transplanted kidneys. Currently, she is studying how suppressing production of the TIM-4 molecule can help block rejection of transplanted organs.34
Looking Ahead
While the research is promising and holds out hope, the reality is that for the foreseeable future, kidney disease is going to be with us. In fact, one recent study showed that early-stage chronic kidney disease is being diagnosed at historic rates.35 But, there are more treatments available than ever before to alleviate patient pain, to slow the disease’s progression and to provide effective treatment at every stage of the disease. What was once a death sentence is now a manageable condition — no small accomplishment at all.
References
- American Kidney Fund. Kidney Failure. Accessed at www.kidneyfund.org/kidney-disease/kidney-failure.
- Mayo Clinic. Chronic Kidney Disease: Definition. Accessed at www.mayoclinic.org/diseasesconditions/kidney-disease/basics/definition/con-20026778.
- Mayo Clinic. Acute Kidney Failure: Definition. Accessed at www.mayoclinic.org/diseasesconditions/kidney-failure/basics/definition/con-20024029.
- National Kidney Foundation. Kidney Disease: Causes. Accessed at www.kidney.org/atoz/content/kidneydiscauses.
- Centers for Disease Control and Prevention. FastStats: Kidney Disease. Accessed at www.cdc.gov/ nchs/fastats/kidney-disease.htm.
- DaVita. What Are the Causes of Kidney Disease?. Accessed at www.davita.com/kidneydisease/causes.
- Mayo Clinic. Chronic Kidney Disease: Symptoms. Accessed at www.mayoclinic.org/diseases-conditions/kidney-disease/basics/symptoms/con-20026778.
- Mayo Clinic. Acute Kidney Failure: Symptoms. Accessed at www.mayoclinic.org/diseasesconditions/kidney-failure/basics/symptoms/con-20024029.
- National Kidney Foundation. Tests to Measure Kidney Function, Damage and Detect Abnormalities. Accessed at www.kidney.org/atoz/content/kidneytests.
- National Kidney and Urologic Diseases Information Clearinghouse. Kidney Biopsy. Accessed at kidney.niddk.nih.gov/KUDiseases/pubs/biopsy.
- Mayo Clinic. Chronic Kidney Disease: Treatments and Drugs. Accessed at www.mayoclinic.org/diseases-conditions/kidney-disease/basics/treatment/con-20026778.
- Mayo Clinic. Acute Kidney Failure: Treatments and Drugs. Accessed at www.mayoclinic.org/diseases-conditions/kidney-failure/basics/treatment/con-20024029.
- American Diabetes Association. Kidney Disease. Accessed at www.diabetes.org/living-withdiabetes/complications/kidney-disease-nephropathy.html.
- Molnar MZ, Kalantar-Zadeh K, Lott EH, et al. Angiotensin-Converting Enzyme Inhibitor, Angiotensin Receptor Blocker Use, and Mortality in Patients With Chronic Kidney Disease. Journal of the American College of Cardiology, 2014;63(7):650-658. Accessed at www.medscape.com/viewarticle/821751.
- The Lupus Foundation of America. Lupus Nephritis. Accessed at www.lupus.org/answers/entry/lupus-and-kidneys.
- Medline Plus. Post-Streptococcal Glomerulonephritis. Accessed at www.nlm.nih.gov/medlineplus/ency/article/000503.htm.
- Cleveland Clinic. Goodpasture’s Syndrome. Accessed at my.clevelandclinic.org/health/diseases_conditions/hic_Goodpastures_Syndrome.
- Mayo Clinic. Wegener’s Granulomatosis: Definition. Accessed at www.mayoclinic.org/diseasesconditions/wegeners-granulomatosis/basics/definition/con-20028113.
- Mayo Clinic. Wegener’s Granulomatosis: Treatments and Drugs. Accessed at www.mayoclinic.org/diseases-conditions/wegeners-granulomatosis/basics/treatment/con-20028113.
- The Johns Hopkins Vasculitis Center. Treatment and Course of Polyarteritis Nodosa. Accessed at www.hopkinsvasculitis.org/types-vasculitis/polyarteritis-nodosa/#treatment.
- National Kidney Foundation. Glomerulonephritis. Accessed at www.kidney.org/atoz/content/glomerul.
- Mayo Clinic. Polycystic Kidney Disease: Treatment and Drugs. Accessed at www.mayoclinic.org/diseases-conditions/polycystic-kidney-disease/basics/treatment/con-20028831.
- Genetics Home Reference. Cystinosis. Accessed at ghr.nlm.nih.gov/condition/cystinosis.
- Cystonisis Research Foundation. Cystonisis Treatment. Accessed at www.cystinosisresearch.org/about-cystinosis/treatment.
- Medline Plus. Alport Syndrome. Accessed at www.nlm.nih.gov/medlineplus/ency/article/000504.htm.
- American Cancer Society. Kidney Cancer. Accessed at www.cancer.org/cancer/kidneycancer.
- National Kidney and Urologic Diseases Information Clearinghouse. Pyelonephritis: Kidney Infection. Accessed at kidney.niddk.nih.gov/KUDiseases/pubs/pyelonephritis.
- National Kidney Foundation. Pain Medicines (Analgesics). Accessed at www.kidney.org/atoz/content/painMeds_Analgesics.
- Medline. Ethylene Glycol Intoxication. Accessed at www.nlm.nih.gov/medlineplus/ency/article/000774.htm.
- National Institute on Drug Abuse. Medical Consequences of Drug Abuse: Kidney Damage. Accessed at www.drugabuse.gov/publications/medical-consequences-drug-abuse/kidneydamage.
- National Kidney Foundation. Engineering Kidneys for Treatments and Transplants. Accessed at www.kidney.org/professionals/Benjamin-Freedman-Engineering-Kidneys.
- National Kidney Foundation. Finding New Ways to Control Phosphorus. Accessed at www.kidney.org/professionals/DrChristov_Control_Phosphorus.
- National Kidney Foundation. NKF Research Spotlight: Dr. Sahir Kalim Studies Dialysis and Other Therapies That Could Better Replicate Natural Kidney Function. Accessed at www.kidney.org/professionals/NKF_Funded_Research.
- National Kidney Foundation. Working to Stop Rejection. Accessed at www.kidney.org/professionals/DrMcGrath_Stop_Rejection.
- Johns Hopkins Medicine. Chronic Kidney Disease Research. Accessed at www.hopkinsmedicine.org/gim/research/content/ckd.html.